This story is a collaboration between Public Health Watch and the Investigative Reporting Workshop.
In April 2008, Jonathan Agin’s 27-month-old daughter, Alexis, was diagnosed with DIPG, a rare brain tumor. Agin, then a civil defense lawyer in Washington, DC, was dislodged from his comfortable life and dragged into the surreal world of a young cancer victim’s parent: The sleepless nights in the din of a hospital, the grueling clinical trials.
“I always had hope,” Agin said in a recent interview, though he knew most DIPG patients survive no more than two years after diagnosis.
Alexis lived for 33 months after her tumor was found. Toward the end of her life, she was unable to walk or speak. She died at 3:03 p.m. on Jan. 14, 2011.
“My knowledge back then of children with cancer was watching St. Jude and Ronald McDonald House commercials,” Agin said. The image of a “smiling, bald-headed kid living happily ever after” was cruelly misleading, he learned, when it came to intractable cancers like DIPG, short for Diffuse Intrinsic Pontine Glioma.

Alexis.
(Photo courtesy Jonathan Agin)
While children with a diagnosis like Alexis face almost insurmountable odds, death rates for many childhood cancers have gone down, thanks to advances in treatment. But incidence rates—the number of cancer cases per 100,000 children—increased 43 percent from 1975 to 2018. While there’s no clear explanation, some experts suspect environmental contamination has played a major role.
“These increases are too rapid to be due to genetic change,” pediatrician Philip Landrigan wrote in a report last year for the Childhood Cancer Prevention Initiative, a collaborative that includes the Children’s Environmental Health Network, the American Sustainable Business Council, and other organizations.
“They cannot be explained by increased access to medical care or by improvements in diagnosis,” wrote Landrigan, director of the Program for Global Public Health and the Common Good at Boston College. His theory is that exposure in the womb or early childhood to chemicals is driving the trend. “Recognition is growing that hazardous exposures in the environment are powerful causes of cancer in children,” he wrote.
When it comes to drug development, children with cancer—defined as people under the age of 20—have long been at the back of the line. There simply aren’t enough of them to inspire massive investment. In 2018, the most recent year for which complete data is available, 15,178 children in the United States were diagnosed with cancer and 1,841 died, according to the Centers for Disease Control and Prevention. By comparison, 1.7 million adults were stricken and 599,265 died.
Now comes the realization that some or many of the 86,000 chemicals used at one time or another in the U.S. may be having an outsize effect on the very young. Few of those chemicals have been tested for safety.
“The American public loves treatments, loves magic fixes,” Landrigan said in an interview. “The rising incidence is not a good-news story. There are no heroes.”
In April 2010, the President’s Cancer Panel, an advisory group created by Richard Nixon in 1971, issued a groundbreaking report highlighting what it called the “growing body of evidence linking environmental exposures to cancer.”
The panel concluded that “the true burden of environmentally induced cancer has been grossly underestimated. With nearly 80,000 chemicals on the market in the United States, many of which are used by millions of Americans in their daily lives and are un- or understudied and largely unregulated, exposure to potential environmental carcinogens is widespread….The American people—even before they are born—are bombarded continually with myriad combinations of these dangerous exposures.”
A co-author of the report was Dr. Margaret Kripke, who founded and chaired the Department of Immunology at The University of Texas M.D. Anderson Cancer Center in Houston. The panel had already looked at lifestyle factors, such as nutrition and smoking, and turned its attention to the environment because of public interest in the topic, Kripke, now retired, said in an interview.
“I was not that enthusiastic about this in the beginning,” she said. “It was controversial, unclear what we’d advise the public to do.”
Kripke’s opinion changed as she worked on the report in 2008 and 2009. “It was truly the most eye-opening experience for me,” she said. “I learned how little attention had been paid to this issue for a very long time.”
That inattention comes in part because “childhood cancers still make up only 1 percent of the cancer diagnoses in the US,” said Dr. Philip Lupo, an associate professor at Baylor College of Medicine in Houston and a genetic epidemiologist at Texas Children’s Cancer and Hematology Center. “That creates a challenge for epidemiologists, who often need large sample sizes.”
Lupo and a colleague at Baylor, Dr. Michael Scheurer, have begun collecting biological specimens, such as saliva samples and primary teeth, from newly diagnosed patients and administering questionnaires to their parents in hopes of identifying novel risk factors for cancer development.
“As we see this explosion in environmental chemicals in human populations, it’s entirely likely they’re playing an important role in the increased incidence of childhood cancer,” Lupo said. Some, such as benzene, a solvent and an ingredient in gasoline, have been shown by occupational and/or animal studies to cause DNA damage, a precursor to the disease.
It’s unlikely genetics are behind the rising numbers, Lupo said, “because genetics don’t work that quickly.”
Congress created a body to investigate possible connections between chemical exposures and illness as part of the Superfund legislation in 1980. But the Agency for Toxic Substances and Disease Registry, part of the CDC, has never achieved widespread credibility.
In 1992, the Environmental Health Network and the National Toxics Campaign Fund released a report accusing the agency of conducting poorly designed studies “used by polluters and government officials to mislead local citizens into believing that further measures to prevent toxic exposures are unnecessary.”
That criticism is still valid, said Stephen Lester, science director at the Center for Health, Environment and Justice, a research and advocacy organization in suburban Washington, DC. The disease registry, known as the ATSDR, relies on existing data—generated, for example, by a state environmental agency—that is often incomplete and of little value for assessing health risks.
“The conclusions are always limited by the data,” Lester said. “Even if the agency could determine that a health cluster exists—and I’ve seen them do that maybe two times out of hundreds of cases—they cannot determine what’s causing the cluster.”
In an emailed statement to Public Health Watch and the Investigative Reporting Workshop, the CDC said, “While we know that chemical exposures can contribute to a variety of health issues and we continue to learn more about these pathways, determining a causal relationship from community-based chemical exposures to specific cases of cancer is rare.”
The ATSDR is being stretched thin, having seen its “purchasing power eroded by relatively flat funding levels despite increasing demand for support in responding to environmental exposures,” the statement said.
The agency received $4.5 million from Congress in recent years to update its guidelines for investigating cancer clusters. The money came from the Strengthening Protections for Children and Communities from Disease Clusters Act—better known as Trevor’s Law, after Trevor Schaefer, who was diagnosed with medulloblastoma, a form of brain cancer, when he was 13 and living in McCall, Idaho, a small town north of Boise.

Schaefer and his mother, Charlie Smith, believe his illness was triggered by waste from an abandoned mine that wound up in the lake that supplied McCall’s drinking water. Five children in the town of 1,700 developed brain cancer within nine months of Schaefer’s diagnosis in 2002, but state health authorities said they found no evidence of a cluster.
Smith won the ear of then-Senator Barbara Boxer, D-California, who introduced Trevor’s Law in 2011. The bill languished and was finally signed into law by President Barack Obama in 2016. Schaefer said he’s grown increasingly impatient with the ATSDR’s failure to finish updating the guidelines in the five years since.
“While the federal government drags its feet and fritters away essential funding, our children are dying,” he wrote in an email to Public Health Watch.
The CDC said it has been using the funds to review the scientific literature, convene an expert scientific panel to discuss best practices, and meet with community members and organizations to hear their concerns.
“Concurrent with efforts to update the guidelines are projects aimed at making county-level cancer rate data more readily available and a pilot effort to determine the utility of electronic health records to provide more timely cancer surveillance data,” the agency said.
In an interview, Schaefer, who runs the Trevor’s Trek Foundation, said, “We’re frustrated. When we talk to parents around the country, they’re getting frustrated. It doesn’t seem like it should take this long.”
In 1942, the Industrial Hygiene Foundation of America presciently advised, “Every new chemical or product should be investigated as to its toxicity before it is prepared in large amounts and released to the public.” Twenty years later, in her book Silent Spring biologist Rachel Carson warned about the overuse of DDT and other pesticides. “If we are going to live so intimately with these chemicals, eating and drinking them, taking them into the very marrow of our bones—we had better know something about their nature and their power,” she wrote.
President John F. Kennedy read excerpts of the book in The New Yorker and was so shaken he established a special panel to investigate Carson’s dire predictions. The panel’s report in May 1963 validated Carson’s findings and bolstered her credibility, which had come under fierce attack by the chemical industry.
Silent Spring generated momentum for the creation of the Environmental Protection Agency in 1970 and the phaseout of DDT. But the chemicals kept coming. By 1976, the year Congress passed the Toxic Substances Control Act (TSCA) in an attempt to require safety testing, more than 60,000 of them were on the market. They were grandfathered in—assumed to be safe unless the EPA could demonstrate otherwise.
This proved to be too great a burden. The EPA has restricted only a handful of chemicals that were in commerce before 1976, including certain forms of asbestos, hexavalent chromium, dioxin-contaminated wastes, and the paint-stripper methylene chloride.
Congress amended TSCA in 2016 in part to shift the burden of proof from the EPA to chemical manufacturers to demonstrate new chemicals are unlikely to present “unreasonable” risks to human health or the environment before being allowed onto the market. During the Trump administration, however, new-chemical reviews by the agency were undermined by unrealistic assumptions that made substances appear safer than they probably were.
“Reviews of existing chemicals were also undermined by tenuous assumptions and illegal exclusions of certain sources of exposure, including environmental releases—of particular relevance to fenceline communities,” said Dr. Jennifer McPartland, a senior scientist with the Environmental Defense Fund.
The Biden EPA has worked to repair the damage but is still way behind. As of August, the agency’s TSCA inventory had climbed to 86,607 chemicals, 41,953 of which were considered “active”—manufactured or processed in recent years.
“EPA has to assess the risk of each and every one of those [active] chemicals, but it’s doing so at about 20-something a year,” McPartland said. Each risk evaluation is supposed to take 3 to 3 ½ years.
The math—nearly 42,000 chemicals and only 20 reviews a year—doesn’t bode well for public health.
“It’s the reality of a lack of regulation for decades,” McPartland said.
On top of all this, the EPA must assess new chemicals before they go on the market. The agency says it has finished 3,394 of these assessments since TSCA was amended, though not every assessment results in a requirement to test. McPartland said this program is also flawed. It’s needlessly opaque, she said, and its managers accede too often to companies’ demands for quick decisions.
In a June press release, the EPA said it had taken steps to bolster risk evaluations underway on 10 high-priority existing chemicals, including methylene chloride and 1,4-dioxane, a solvent found in paints, cosmetics, detergents, and other products that have contaminated drinking water in some parts of the country. The agency said it would take into consideration “exposure pathways,” such as air and water, that had been disregarded by the Trump administration. The aim is to “restore public trust, provide regulatory certainty, and, most importantly, ensure that all populations that may be exposed to these chemicals are protected,” the EPA’s assistant administrator for the Office of Chemical Safety and Pollution Prevention, Michal Freedhoff, was quoted as saying.
In a written statement responding to questions from Public Health Watch and the Investigative Reporting Workshop, the EPA said it found “risks across many uses of these chemicals and will be proposing rules to protect against these risks beginning in 2022.” The agency said it has begun working on the next 20 evaluations.
The health impacts of cancer-causing chemicals land heaviest on low-income communities and communities of color, said Nsedu Obot Witherspoon, executive director of the Children’s Environmental Health Network. In such places “people who are doing all the right things—you know, taking care of their children the best they can and sending them to school and working hard”—face carcinogenic exposures from industrial facilities, heavily traveled highways, and other polluting sources.
Witherspoon was born in 1975, the year childhood cancer incidence began rising. “That shows you, right there, it’s not genetics only,” she said. “There’s something else happening that is making young, young children predisposed. Childhood leukemia and certain brain cancers and tumors and whatnot are very much, sadly, related to certain levels of exposure. When you look at young children, they’re not smoking, they’re not drinking.”
Some in the private sector aren’t waiting for government intervention. In 2013, two students at the Helen R. Walton Children’s Enrichment Center in Bentonville, Arkansas, were diagnosed with cancer. The illnesses were determined to be non-hereditary, and suspicion fell on chemicals the children might have ingested, inhaled, or absorbed in their daily lives.
“It made us think twice about what we could be doing better,” said the center’s executive director, Michelle Barnes. “I was just horrified to hear about what is in our furnishings and carpets and things like sealants and non-stick cookware.”
The campus, which opened in 1982, was already marked for replacement. After the students’ cancer diagnoses, Barnes, other members of the center’s leadership team, and its board of directors were determined to do things differently. New York-based LTL Architects was deemed to have the right sensibility and was hired in 2016. The new, $18 million campus opened in May 2019 with a 50,000-square-foot building that houses 244 students ages 5 and younger.
“We eliminated or significantly reduced exposures to six major classes of chemicals,” Barnes said, including a group of “forever chemicals” known as PFAS. Food is no longer stored in plastic bowls covered with plastic wrap, which can leach hormone-disrupting phthalates and bisphenol-A. Instead, it’s kept in stainless-steel bowls with lids made of medical-grade silicone. Teethers are natural rubber, not plastic.
Twelve million children 5 or younger are in some form of child care in the United States. Barnes said she’s heard from parents, school administrators, and developers interested in replicating what the Children’s Enrichment Center created.
“We want to use this as a model for the early-childhood industry as a whole,” she said.
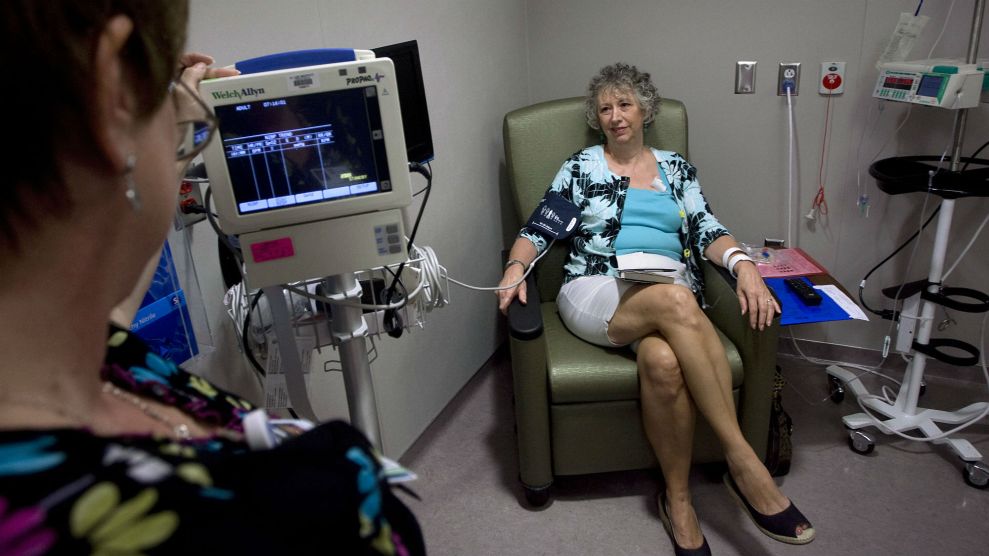
For the foreseeable future, thousands of children will continue to be diagnosed with cancer each year and require treatment. But unless the drug-development process undergoes a significant transformation, they will remain a lower priority than adults.
Promising therapeutics for children have a difficult time moving from concept to commercial viability, said Vickie Buenger, president emeritus of the Coalition Against Childhood Cancer and mother of Erin Buenger, who died of neuroblastoma at age 11 in 2009.


Erin Buenger.
“The children fall through the cracks because it’s tough to develop drugs for very small markets,” said Buenger, a business professor at Texas A&M University. The Food and Drug Administration has approved hundreds of cancer drugs, she said, but only six were developed with children in mind.
This disparity forces children to endure a “blast furnace of toxicity” during treatment with drugs designed for adults, she said. “They have to live with the side effects of such harsh treatment for decades.”
Uplifting survival stories create a sense of complacency, said Agin, who left his law practice after Alexis died to lead the nonprofit Max Cure Foundation and later start his own organization, Prep4 Gold. “When the messaging is, ‘Look how great we’re doing,’ that drives the lack of haste in developing new therapies,” he said.
And survival doesn’t guarantee a normal life. Many childhood cancer victims develop new strains of the disease or suffer other health problems, some related to the treatments themselves. Trevor Schaefer said he suffers from tinnitus in his right ear, double vision, hearing loss, post-traumatic stress disorder, and depression almost two decades after his brain-cancer diagnosis.
A National Cancer Institute spokesman did not respond to written questions intended for one of its pediatric cancer experts. Instead, he referenced a September blog post by institute director Dr. Norman Sharpless, who touted the progress that has been made. Treatments have become more precise, leading to better outcomes, Sharpless wrote. Today, for example, roughly 90% of children diagnosed with acute lymphoblastic leukemia are cured; a half-century ago the disease was almost always fatal.
Responding to lobbying by the Coalition Against Childhood Cancer and other groups and individuals, Congress has tried to improve the odds for children with hard-to-treat tumors, passing the Pediatric Research Equity Act in 2003, the Creating Hope Act in 2011 and the Research to Accelerate Cures and Equity for Children Act in 2017. The bills incentivized, to varying degrees, drug development for pediatric cancers, though one big loophole had to be closed.
The legislation has shown “the beginnings of value,” Buenger said. All six of the child-focused oncology drugs approved by the FDA came into use after the bills were passed.
Gregory Reaman, a pediatric oncologist and associate director for oncology sciences at the FDA’s Center for Drug Evaluation and Research, cautioned that there are still “major challenges to cancer drug development in children because many of the cancers that are most difficult to treat and that remain as major problems from the standpoint of not having effective therapies are driven by molecular abnormalities that are very, very different from the molecular abnormalities that cause adult cancers.
“I think kids are at the back of the line because the laws have not allowed them to be at the front of the line, where they belong,” Reaman said. “So, that is now changing, and we’ll have to see if the change in the laws actually does live up to the promises…”
Peter Adamson, who leads cancer drug development at Sanofi, a global pharmaceutical company, said researchers’ understanding of childhood cancer has advanced, especially over the past decade, “and that understanding is now helping to drive research.”
Still, he said, cancer remains “the leading cause of death from disease” in children.
“I think the community continues to look for the right balance of requirements and incentives to help catalyze drug development,” Adamson said.
Buenger acknowledged the work of “good actors” in the private sector. In November, for example, a firm called Oncoheroes Biosciences Inc. announced it had agreed to license a drug called volasertib, which shows promise in treating acute myeloid leukemia and rhabdomyosarcoma, a type of soft-tissue cancer, to Notable Labs Inc. The former will have the right to commercialize the drug for use on children, the latter for use on adults.
But Buenger isn’t ready to declare victory.
“It’s a process, and we don’t want it to be just performative,’ she said. “We’re not going to be satisfied by people saying, ‘We’re trying.'”
Jim Morris is executive director and editor-in-chief of Public Health Watch, a nonprofit investigative news organization. Lauren Berryman is a reporter with the Investigative Reporting Workshop, an independent, nonprofit newsroom based at American University’s School of Communication.