A mother holds her trans son's supply of medication.Rory Doyle/The Washington Post/Getty
Countless words have been spilled—including in Mother Jones—on the topic of medical care for transgender youth. The attention, in part, comes from a steep jump in the number of teens who self-identify as transgender in surveys—and, even more significantly, by the massive, coordinated, right-wing campaign designed to politically weaponize transgender kids’ very existence.
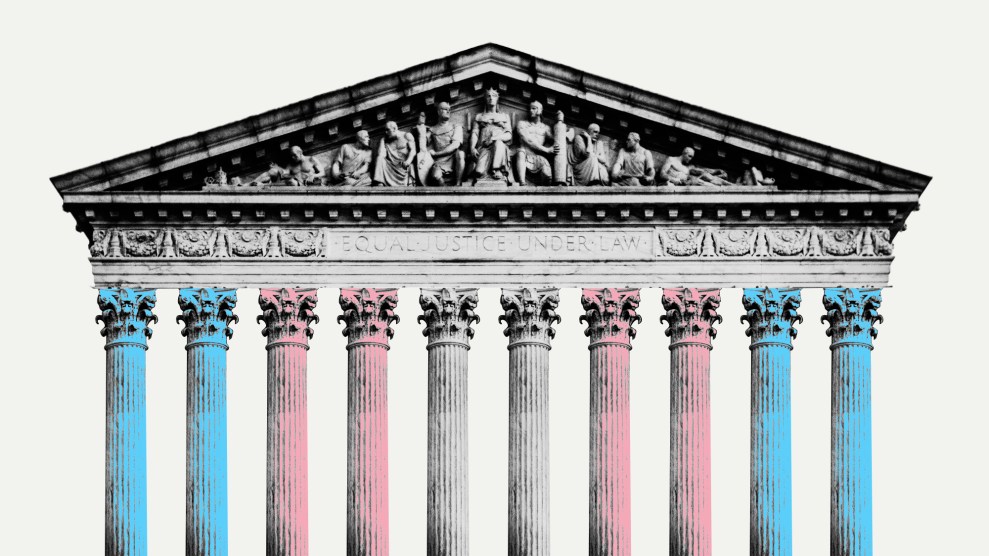
At least 373 bills attacking transgender health care, usually for minors, were introduced in statehouses over the past two years, according to the Trans Legislation Tracker. Add to this the campaign promises by incoming President Donald Trump to “end child sexual mutilation” that were further amplified by $200 million in anti-trans political advertising this election cycle. By June, the Supreme Court is expected to decide if states can unilaterally ban gender-affirming medicine for trans minors.
Amid all the distortions, it has been difficult to determine how many young people are actually receiving gender-affirming treatments.
So, Jae Corman, the head of research and clinical analytics at Folx Health, a major LGBTQ telemedicine provider, teamed up with Harvard researchers to find out. “All the media that has been coming out has been saying, ‘So many youth are being rushed into care, and there are just so many youth accessing gender-affirming care,'” Corman says. “We said, ‘Okay, let’s look at a claims database.'”
The researchers analyzed insurance claims data for 5.1 million youth who fell into the 8–17 age bracket at any point between 2018 and 2022. Then they looked at how many had been coded as transgender by a medical provider and received gender-affirming medications.
Their findings, published on Monday in a peer-reviewed research letter in JAMA Pediatrics, offer a crucial reality check. Their findings? Just 0.017 percent of youth were coded as trans and received puberty blockers. And just 0.037 percent were trans and accessed hormone therapy.
“There’s a lot of attention being spent on an issue that only affects a very, very, very tiny part of the population.”
All told, that’s about one-twentieth of one percent. “There’s a lot of attention being spent on an issue that only affects a very, very, very tiny part of the population,” Corman says.
Both puberty blockers and hormone therapy have been associated with improved mental health, including fewer thoughts of suicide, for trans teens—which is why they’re supported by the American Academy of Pediatrics and other leading US and international medical associations. Puberty blockers, for instance, temporarily inhibit the development of secondary sex characteristics, like breasts and periods in those assigned female at birth, or facial hair and Adam’s apples in those assigned male at birth—physical changes that can cause clinical levels of distress for youth with gender dysphoria. As trans teens get older, hormone therapy is used to spur the development of secondary sex characteristics associated with the opposite biological sex.
Yet the new research paints a picture of how rarely trans minors are given those medicines. Even among youth with a trans-related diagnosis, only 5 percent were on puberty blockers, and 11 percent were on hormone therapy. Not a single patient under the age of 12 took hormones, among the 5.1 million-person sample.
That’s a huge gap—made even starker by how rarely kids ever received a trans-related diagnosis code from one of their providers. Only about 0.34 children in the database had a diagnosis related to gender dysphoria. That’s far fewer than the 3.3 percent of high schoolers who self-identified as transgender in a 2023 CDC survey. According to Corman, the gap can in part be explained by patients and families choosing not to pursue a diagnosis or medical treatments. Much of the rest can be attributed to how hard it is for young people to access gender-affirming care—contrary to the claims of anti-trans politicians. “First,” Corman explains, “there’s having a parent or caregiver who believes you enough to take you in for care. Then, even among all the well-meaning parents, they often don’t know where to go. There might not be a place in their area.” Out-of-pocket costs can be high, even with insurance. And, waiting lists can be extremely long among providers who do offer care to minors.
Crucially, the research looked at the five years before any state bans on gender-affirming medications for minors took effect. Since then, about half of states have made it illegal for doctors to give minors with gender dysphoria hormone therapy or puberty blockers. And yet, the same medications remain available for cisgender minors, who use them for precocious or late-onset puberty, though the researchers did not analyze how often they are prescribed.
The new data does not reflect uninsured people or those on state Medicaid plans, which generally do not cover gender-affirming treatments for minors. But they also don’t include people who pay out-of-pocket for care, because their insurance doesn’t cover it. Yet if anything, the new numbers likely overestimate how often youth received gender-affirming medications, according to the researchers. That’s because the database they used included only people on private, large-group insurance plans. “Think of it as the most privileged commercially insured populations,” Corman says. “These are the children who get the best access to care.”