Tanya Haj-Hassan examines wounded children at a hospital in central Gaza in March.Abdel Kareem Hana/AP
On Tuesday morning, as the party coalesced around Vice President Kamala Harris at the Democratic National Convention, doctors spoke at a press conference in Chicago about what they witnessed in Gaza since last October as volunteers. At many points, their testimony proved unbearable.
Tanya Haj-Hassan, a pediatric intensive care doctor, described treating children with no surviving relatives—a situation so common an acronym has been needed in the hospitals: WCNSF (Wounded Child, No Surviving Family). She told the audience about holding hands with children as they breathed their final breaths.
Uncommitted delegates to the DNC have been pushing for Haj-Hassan to be able to speak from the main stage of the convention. But, so far, national Democrats have not agreed to that request.
I interviewed two of the doctors after the event. Dr. Ahmad Yousaf is an internist and pediatrician from New Jersey who now practices in Arkansas—primarily in the intensive care unit. He volunteered at the Al-Aqsa Martyrs Hospital in Gaza for three weeks in June and July. Dr. Nabeel Rana is a vascular surgeon in North Carolina who overlapped with Yousaf at the Al-Aqsa hospital. They did not know each other before meeting in Gaza, but quickly developed a bond born out of shared trauma.
This interview has been edited for length and clarity.
We’ve seen the images on social media and elsewhere of the scale of the destruction in Gaza. How did that compare with what you saw firsthand?
Dr. Rana: There are no words, pictures, or videos that can really capture what’s happening. As soon as we got to the other side of the Gaza border crossing, it was like this dystopian image out of a movie. I mean it was just dust. It was an annihilation of the entire land. It’s not just buildings that were destroyed. There were things that looked like dirt fields, but I was told, That was an orchard. That was this farm.
Going from the border to our hospital in the middle segment of Gaza, there was nothing normal, no building untouched. Everything was decimated for miles and miles. It wasn’t like this was a target, that was a target. It was like someone steamrolled through the entire city.
Dr. Yousaf: It felt like we were entering a post-apocalyptic movie scene, or a Mad Max world where none of the roads were drivable and none of the homes were habitable. There were people strewn across the streets in tents because that’s all they had. There were others living within the rubble of homes because it was better to have something over your head even if it was completely unstable.
Initially, I thought that it was going to be what we saw on the news and Telegram and Instagram. But when we got there, the devastation was so much worse than I could have imagined was possible in the period of time that this war has been going on.
What were conditions like inside the hospital?
Dr. Yousaf: To call it a hospital at that point was kind of a stretch. It was serving as a temporary shelter for at least half the people on the property. There were tents in and around it. Even within the hospital, the hallways were full of families because they knew that it was a building that was relatively protected.
It was an obstetrics hospital before the war, but it became a trauma ward. The place wasn’t meant to take care of trauma patients. They had three operating theaters and two delivery rooms had been modified into operating theaters. But they were not truly capable of taking care of those kinds of patients.
I watched Dr. Rana do a surgery in which the lights went out multiple times. That was common. The ventilators in the ICU would go out of oxygen. You were just trying to survive and keep people alive in the short term. It didn’t function like any other medical facility I’ve ever been in.
Dr. Rana: It’s a small hospital. Now it’s all over the news and it seems like this big medical care center, but it’s a tiny hospital. The day we arrived there were 700 patients in a 200-bed facility.
The hallways were just packed with people. You don’t know who’s a patient and who’s not—other than one is missing a limb. There’s no air conditioning. The hospital is running on generators because there’s no electricity. Those generators start and stop.
People in there were just suffering 24 hours a day. All the time. There was just no way just to give them even brief relief.
From a surgical standpoint, there are no supplies. There are no gowns. You don’t have the right instruments. You do a surgery, then you don’t have the right sutures to close those wounds. Everything is just damage control all the time. You can’t ever step out of that mode to where you can actually start helping someone heal—to where they can actually start recovering.
The staff would say that if there’s a couple days where the bombing is minimal and massive traumas are not coming in, we try to get patients out of the hospital to open up space—not even beds—for the next onslaught of patients. Dr. Yousaf and I were there long enough to witness that cycle multiple times.
What would happen during a mass casualty event?
Dr. Yousaf: First, there is the constant buzz of drones above our heads. It sounds like your neighbor is mowing their lawn. You also hear artillery shells or bomb blasts. But if it was close enough—if we felt the earth shake under us or if the building moved—we knew that we’d be getting the patients from that bomb blast 30 or 45 minutes later. They’d often come in on donkey carts and ambulances and other vehicles. Or they’d just be carried in their arms by family or community members.
They would rush into the OR in panic while their family member was dead or dying. We’d say: Put them over there on the floor because we don’t have space anymore. And there could be 16,17,18 people coming in like that consecutively.
We’d really try our best. And by we, I really mean the Gazan medical staff. They would be saying: That person’s not going to live. Leave them there. That person is dead already. Here’s the people we can try to save.
Gloves were a luxury. We were using hemostats to pull shrapnel out of people, and we’d have to pour Betadine on it between patients because we didn’t have enough sterilization to go around. Every mass casualty event overwhelmed the system. Right when you felt like you were catching up, there was another explosion and you knew that more people were coming.
What was available in terms of painkillers and anesthetic?
Dr. Yousaf: We had one medicine, ketamine, that prevented a lot of misery. It’s a sedative medicine we would never use in any other environment in the way that we used it there.
People came in with legs torn off and their skin burned off and visible bone-crushing wounds. Dr. Rana and I saw a 10-year-old who came in with no pelvic bone. The only relief we could give was to push ketamine—hoping it would sedate them until we had time to really assess what was going on. In the long term, we had very little to nothing. Outside of the trauma room, we were using ibuprofen and Tylenol often for full body skin burns.
Dr. Rana: People in there were just suffering 24 hours a day. All the time. There was just no way just to give them even brief relief.
As a surgeon used to working in an American hospital, what was it like to be in such a helpless position?
Dr. Rana: You heard some of this before you went so I was familiar with a bit of it. But when I got there, it was a very steep learning curve. Nothing is normal. Nothing is what you’re used to having here.
It was very humbling because in the very beginning I was learning from Gazan medical workers. They had been doing this for months. The physicians and surgeons there would use their phones as OR lights when the lights went out. They were using instruments that should not normally have been used for the things that we were doing, but they just kept going. One of our colleagues, a surgeon from Australia, did an entire colon resection without electrocautery, which we use for controlling bleeding during surgery.
Maybe you didn’t have lights. Maybe you didn’t have suction. There were all these things that would absolutely halt an operating room here because you can’t give quality care without those things—at least with what our standard is. But over there, you don’t have a choice.
During the press conference, you mentioned a pregnant woman you treated up until her death. What happened?
Dr. Yousaf: The first day I was in Al-Aqsa hospital, there was a mass casualty event. I want to say 15 or 20 people came in simultaneously. She was plopped down right next to me—belly down, initially—with full burns. Her hair had been burned away. Her face was completely burned. Seventy percent of the surface area of her body was burned. And the first thing we noticed during our primary survey, which is the kind of first quick glance, is that she had shattered her leg from an explosive injury. I could see the tendons.
Then we heard screaming in Arabic outside the door saying, She’s pregnant. She’s pregnant. It took me a minute to really process what they were saying because you couldn’t tell this patient’s age due to the burns. When we realized what was happening, we flipped her over and somebody put an ultrasound on her belly and noticed that she had a viable, kicking, 18-to-20 week old pregnancy.
When you hear of a pregnant lady, everybody’s sensitivity gets even sharper and we did what we could. She was rushed to the OR, got the orthopedic surgery, got taken care of. She ended up undergoing an amputation of the leg because there was no way that it was savable.
But every single doctor and nurse and health care provider realized an inevitable reality; she was going to die.
She ended up in the ICU for many days, where I cared for her as part of a team. Every day on rounds, we would pass by her bed. She moaned and groaned in pain the entire time. We could only provide her relief intermittently with very, very inadequate medications until the day came where we rounded on her and she was no longer in the bed. We all knew what that meant. The nurse said to me in Arabic that it was a mercy—for her and for her husband, who was with her the entire time. The guy never left her bedside. He watched her suffer. She suffered. And there was no happy ending there.
There are so many stories of the Gazan people that don’t have a happy ending. In the privilege we live in, we imagine: Yousaf is going to say that the baby was born and the baby lives on. No, no. The baby died. Her mother died. Her husband is now a widower with a lifelong trauma that he’ll never be able to overcome.
I don’t know if there are other family members. I don’t know who else died in the explosion.
In many cases, the bombs causing these injuries and deaths were likely made in America. And in some cases, the weapons may have been paid for by American taxpayers. How does that connect to your decision to come to Chicago?
Dr. Rana: There’s a lot of talk about ceasefire, and what everyone needs to understand is that we’re so far past the point of where a ceasefire should have happened. There’s so much destruction, death, devastation, annihilation, genocide, all of these things have continued to happen under our watch.
What we’re telling you as Americans who were there on the ground is that innocent people and an entire society is being decimated. We’re not only standing by and watching it, we are contributing to it. We are actively doing it. And it’s unbelievable to me. I just can’t understand how we continue to supply bombs then talk about a ceasefire. The hypocrisy of it is just astounding.
Was there a consensus among the doctors you were working with that you were witnessing a genocide?
Dr. Yousaf: There was no doubt.
Dr. Rana: Without a doubt.
Dr. Yousaf: I’d love to meet a doctor who was there for more than seven days who would say that what they saw wasn’t a genocide.
Dr. Rana: In terms of war crimes and things like that, we saw targeting of children. We saw young men targeted with rifle shots to their thighs to try to require amputation of their legs.
There were quadcopters targeting men in their groins and genitals. They would come in with no other injuries and would lose their testicles. They’re healthy young men, but they’ll never have kids. One of the surgeons I was speaking to said, This is the seventh one like this I’ve seen. This is something they do. A quadcopter comes in and just targets a young man.
I asked the urologist who was doing the operation, How many of these have you seen?
Too many to count, he said.
The reason I believe him is that when he finished reconstructing this young man, I was so amazed at his proficiency. This was obviously somebody who’d done a ton of this type of case. Either you’re trying to decimate the future of a society, or it’s just sick entertainment for sociopaths. And I don’t know which one it is.
Have you ever gotten involved in politics like this before?
Dr. Rana: No, I haven’t. I went with an organization called Humanity Auxilium and the founder of that organization is very active in medical aid and relief. We had a discussion before I went and she said that as physicians, when we go to these places, you also have to be an advocate. I told her that I’m not a public speaker. I’m not a politician. I’m just a physician who has a set of skills. I’m going to go there and do what I can do and help people, and that’s my role.
But the one thing that everybody there asked was: Please, go back and tell everybody about us. They didn’t ask for help. They didn’t ask for anything other than that they don’t want to be forgotten and neglected. And so the responsibility I feel is to tell what I saw. I also feel an obligation to speak out because the hypocrisy is not just on our country’s part but on our side, too. I paid for those missiles that were being used there. My tax dollars were used to do that.
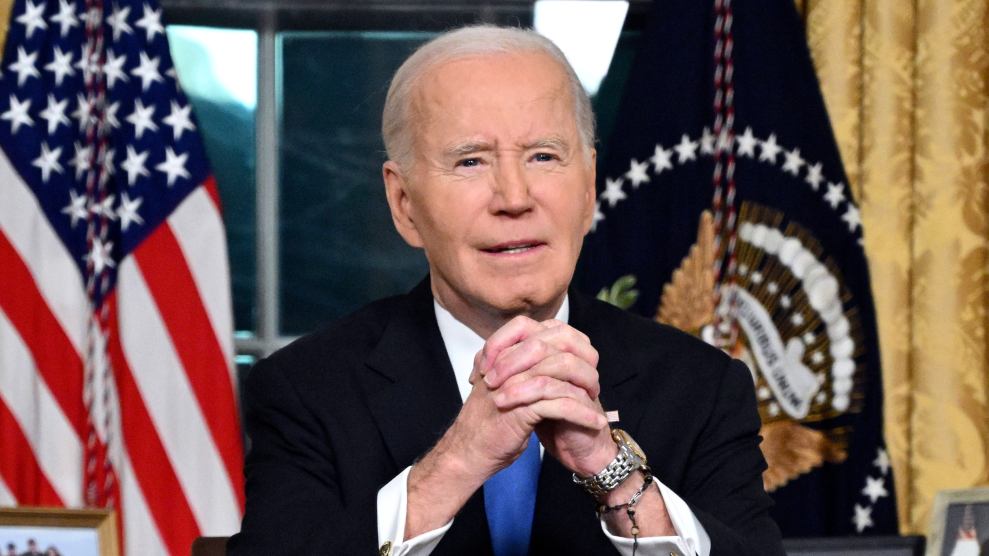
In his convention speech on Monday night President Biden said he’s been working around the clock to surge humanitarian aid and secure a ceasefire. What’s it like to hear that?
Dr. Yousaf: I’m going to curse here, but that’s bullshit, right? It’s bullshit because you can only judge somebody by what they’ve done. Words mean nothing anymore. Gazans over there showed us what humanity and human dignity mean in an environment where they are being treated inhumanely and without dignity. Nobody should get away with sleeping comfortably at night knowing that they can say one thing on one side and then do something else on the other.
What are the most important steps you want to see the United States take?
Dr. Yousaf: We’re not politicians and we’re not military strategists so I don’t know what all the steps are. But the basic steps are pretty simple: Let’s stop sending bombs to people who are using them to kill children and civilians. Let’s allow open access to medical supplies, humanitarian aid, and international news agencies so we can have more witnesses than a couple of doctors. And let’s allow for an environment where we treat the Palestinian people like they deserve: as human beings who deserve the same rights as and the same access to humanitarian aid and health supplies and health care as the rest of us.