Mother Jones illustration; Boston Public Library/Unsplash
It’s been an unprecedented two years for science, to put it mildly. We’ve seen a new virus spread across the world, entire cities go on lockdown, a devastating 6 million deaths globally (and counting), and in record time, the development of a life-saving vaccine. It’s no stretch to say that for anyone living on Earth, Covid has been a big freakin’ deal.
But during this time, researchers have continued to make progress toward a vaccine for another deadly virus: HIV, a pathogen that has vexed scientists and devastated patients for decades—and which infects more than a million people, including 100,000 children, around the world each year. With the world’s attention on Covid, much of that progress, experts say, has flown under the radar.
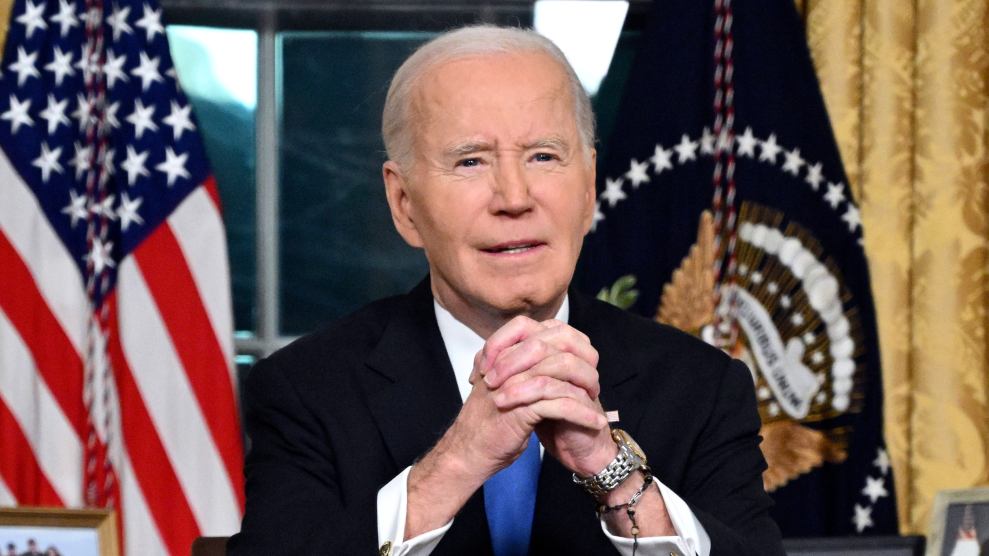
In particular, researchers say they are starting to see promising results with rare, powerful antibodies that can prevent HIV infection—and are working to build vaccines that can get our immune systems to produce those antibodies. While these developments have not yet been “home run, knock-it-out-of-the-park successful by any means,” Dr. Anthony Fauci (yes, that Fauci), who heads the National Institute of Allergy and Infectious Diseases, tells me, they represent “gradual incremental progress”—steps forward in the marathon to an HIV vaccine. Dr. Larry Corey, the principal investigator for the HIV Vaccine Trials Network, a nonprofit funded by the National Institutes of Health to carry out HIV studies, described the field as having “a highway to success.”
A “highway” may not sound like much. But when it comes to HIV—a virus that has proven itself to be a unique, smart opponent—even little wins are significant. In the more than 40 years since the human immunodeficiency virus was discovered, researchers have developed many antiretroviral drugs to fight it, including drugs that can suppress the virus and keep AIDS under control. Some of these drugs can also prevent HIV infection and can be administered in the form of pills, a vaginal ring, or as of late last year, long-lasting injections. But a vaccine, frustratingly, has remained out of reach.
There are several reasons why this is the case. For one, the virus is among the most diverse life forms on Earth. While an individual with Covid may produce one or two variants of the virus during the 10-15 days they’re infected, Corey says, an HIV-infected individual will see about 100 new variants per day, for as long as they are infected, a period which can span decades. So the virus can look vastly different from person to person across the world.
Another challenge is that our immune systems can’t stop HIV—at least not on their own. With Covid, for comparison, researchers observed early in the pandemic that if people got infected, the vast majority would make an immune response to the virus and recover. “We knew that if we made a vaccine that was as good as natural immunity,” Corey says, “that would be likely to be effective.” But with HIV, almost no one clears the infection. “The human immune system can’t eliminate it,” Corey says. In short, it’s difficult to replicate an immune response that doesn’t usually occur in the body. It’s sort of like trying to perform a concerto—without knowing how to read music.
And once HIV gets into our bodies, it’s there for life. So a vaccine can’t just provide just some immunity. Unlike, say, the Covid vaccine, which can help protect against severe illness in the case of a breakthrough infection, an HIV vaccine has to provide a total immunity shield. “This vaccine has to do something no other vaccine has ever successfully done yet,” Dr. Barton Haynes, who directs the NIH-funded Center for HIV/AIDS Vaccine Immunology and Immunogen Discovery at Duke University, tells me. “And that is to 100 percent protect against infection. Because once infection occurs, then the vaccine has failed.”
So, if researchers do manage to create an HIV vaccine that works, it has to clear several complicated hurdles. It will have to A) offer broad protection against an enormous number of variants; B) teach our bodies how to do something we don’t normally do on our own; and C) do this in such a way that offers total immunity. It’s largely because of these challenges that we don’t have an HIV vaccine today, and in part why several major clinical trials for potential vaccines have been unsuccessful; for every strategy we’ve thrown at HIV, the virus has found a way around it.
“It’s the Holy Grail of vaccines,” Haynes says.
The good news is, after spending years learning how HIV works (and enduring repeated clinical failures), many leading HIV researchers I spoke with say they have finally singled out—and tested—the right tool to fight the virus: rare, powerful antibodies known as “broadly neutralizing antibodies,” or bnAbs. Some people produce these antibodies after years of infection.
In general, infection-blocking antibodies work like this: When a virus enters your body, antibodies recognize and attach themselves to proteins on the surface of viruses, preventing those pathogens from entering our cells, and protecting us from getting sick. But because HIV mutates so easily, the virus’ surface can look pretty different between variants, making it difficult for antibodies to keep up. There are, however, a few parts of the virus that don’t change much between variants, like the virus’ “Achilles heel.” Antibodies that attach to those spots are known as broadly neutralizing.
In early 2021, researchers at the HIV Vaccine Trials Network published the results of two landmark studies that put bnAbs to the test. Across the two studies—known collectively as the “AMP trials”—more than 4,600 participants in North and South America, Europe, and Sub-Saharan Africa were given 10 infusions of a special, lab-manufactured antibody over 20 months. While none of the participants saw complete protection against HIV, the researchers observed that the bnAbs did protect against some strains of the virus—showing for the first time in humans that bnAbs can prevent HIV infection—a “proof-of-concept” for bnAbs, the study’s authors write. When I ask Dr. Steven Deeks, an HIV researcher, clinician, and professor of medicine at the University of California, San Francisco, who was not directly involved with this research, about the significance of the AMP trials, he says, “Without question, it was a major advance.”
Still, what was tested in this trial was infusions of antibodies—not vaccines. The next step would be to make a vaccine that prompts our bodies to produce these superstar antibodies on our own. “We know that [these antibodies] exist,” Corey says, and that across all variants, the virus has about seven different sites of attack that the antibodies can target. “The issue is, how do we design an immunogen—a vaccine—that would actually awaken this?”
Scientists are already working on it. Last year, researchers at Scripps Research announced that they’d created a vaccine that could kick off the process of making bnAbs: When given their vaccine, 97 percent of participants produced immune cells that could make early versions of these antibodies. It was a small, preliminary clinical trial, but the results are promising. (Haynes’ group at Duke is also expected to release the results of a similar trial soon, he says.) “If there’s any big news,” Haynes says, “that’s the news that the field can now do this.”
But again, this is just one of many steps; a truly effective AIDS vaccine will at least take several more years, experts say. When I ask Corey when he thinks the world will finally get there, he says that preventative, broadly neutralizing antibodies may be available (in the form of infusions) in “three to four years.” But a vaccine to actually make those antibodies “may take double that.” When I asked Deeks the same question, he reminded me that back in 1984, President Ronald Reagan’s secretary of health estimated that we’d have an AIDS vaccine in two years. That was nearly 40 years ago. “Since that time,” he jokes, “no one’s ever actually answered the question you just asked, directly.”
However long it takes, experts hope the process will move faster with the help of messenger RNA. If mRNA sounds familiar to you, there’s a good reason why: It’s at the core of the two most widely used Covid-19 vaccines in the US. As you may recall, mRNA essentially works by providing our bodies with a set of instructions to build molecules; with the Covid vaccines, for example, those instructions code for the coronavirus spike protein. But mRNA can be easily tweaked to provide instructions for all sorts of molecules—including ones that can stimulate the production of bnAbs. And unlike, say, making entire proteins from scratch, mRNA can be made quickly and cheaply. “Every time we want to make a different protein, it takes 16 or 18 months and 4 or $5 million,” Corey says. “With RNA, you can make it in 100 days. And costs can be in the hundreds of thousands of dollars.” So with mRNA-based vaccines, experts hope the testing process will be nimbler than it has been in the past.
As a technology, mRNA isn’t new to HIV vaccine researchers. (Back in 2017, in fact, Haynes was among the first researchers to demonstrate the power of an mRNA vaccine, in this case in protecting against Zika in mice and monkey trials.) But Covid’s “big gift” to the HIV field, Haynes says, is that it demonstrated the speed of mRNA. “We knew [mRNA] was going to work when we saw the Zika trials work,” he says, but Covid “showed how fast you can do it.”
When I spoke with Fauci, he was optimistic about mRNA and HIV—the technology saw “amazing success” with Covid, after all—but urged caution. While mRNA could “be a big boon to the [HIV] field,” Fauci says, “It’s too premature to say that this is going to be a quantum advance in HIV vaccinology.”
Hopefully, mRNA will have a chance to prove itself. Some experts worry that with the arrival of drugs that prevent HIV infection, testing potential HIV vaccines will become even more difficult. Ethically, researchers must offer these drugs to study participants in vaccine trials—but if every participant is on medication that prevents HIV infection with high efficacy, it becomes much more difficult to measure how well a vaccine is working, if at all.
Still, even with these drugs available, Fauci says, the search for a vaccine remains a worthy cause. “For good, long-lasting, global protection against an infection like HIV,” he says, “you always have to aim for a vaccine because that would be the optimal level of protection that you would get.” And as Dr. Nirupama Sista, director of research and development for FHI 360, a nonprofit that manages HIV prevention studies, points out, fighting HIV may not require a one-size-fits-all solution. For people living in the shadow of HIV, particularly those in lower-income countries, having many preventative options is key—whether it’s drugs taken as oral pills or long-lasting injections, or a vaccine. “A vaccine, if it is highly efficacious, adds yet another prevention tool in the toolbox,” she says. “And every intervention that we can add helps in reducing infection.”