Around this time last year, we were still living relatively normal lives. Donald Trump had just survived his first impeachment, Bernie Sanders had clinched a victory in the New Hampshire primary, and Justin Bieber had released his first album in nearly five years. Meanwhile, on the other side of the world, China struggled to control its outbreak of a virus we would eventually call SARS-CoV-2. Most of us had no idea how the coronavirus would upend our lives.
Nearly 30 million cases and more than 485,000 deaths later, we’re beginning to see the light at the end of the tunnel. Vaccines are working! Cases are declining! So exciting is this progress that dozens of states are opening back up or loosening restrictions for restaurants, gyms, salons, bowling alleys, and in-person schooling. Great news, right? Not exactly. Actually, we’re now in a situation that’s remarkably similar to where we were exactly a year ago. And experts are warning that now is not the time to let up.
At least three designated “variants of concern” have made their way to the United States: B.1.1.7, which was first identified in the United Kingdom (where it drove a surge in cases), B.1.351, which was first identified in South Africa, and P.1, which was first identified in travelers from Brazil who were tested at a Japanese airport. These variants seem to spread much more easily from person to person—around 50 percent more, researchers estimate in B.1.1.7’s case—and are possibly more deadly, though research is limited.
B.1.1.7 already appears to be spreading rapidly across the country, and it shows no signs of stopping. For a sneak preview of what could happen next, scientists are looking to Denmark: Like in the United States, COVID cases there are currently declining. But unlike in the United States, Danish authorities are sequencing genomes from more than half of the country’s positive cases. As a result, they’ve been able to detect “two epidemics“—one driven by the old variants and receding, and another that’s on the rise, driven by B.1.1.7. (See chart.) Researchers warn that their models indicate a “calm before the storm.”
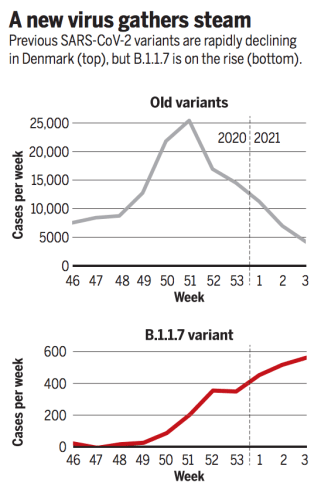
In other words, it’s a crisis waiting to happen. Again.
To better understand exactly what we’re up against with these new variants, I called Joseph Fauver, a genomic epidemiologist and associate research scientist at the Yale School of Public Health, Sarah Otto, an evolutionary biologist and a professor in the Department of Zoology at the University of British Columbia, and John Swartzberg, a clinical professor emeritus specializing in infectious diseases and vaccinology at UC Berkeley’s School of Public Health.
In short, they told me that the variants are a real threat, one that was made possible by the sheer scale of this pandemic. Worldwide, more than 100 million people have been infected by the coronavirus. More cases mean more opportunities for the virus to evolve. That’s why experts say slowing the spread—by masking, social distancing, and when we’re able, getting vaccinated—is still our best option against these variants, as well as future ones. As Swartzberg put it, “We’ve got to get people vaccinated as quickly as possible because we’re in a race to protect people’s lives. But we’re also in a race with evolution of these viruses.”
Here are some things to know about the new variants:
The variants have all found the same “secret sauce.”
Like you and me, the coronavirus isn’t perfect. As it replicates, copying its RNA over and over, it’s bound to make mistakes. These mistakes are called mutations, and most of the time, Swartzberg explains, they don’t help the virus. But over many, many replications, in millions of hosts, one of these “experiments” may be successful, giving the virus a competitive edge over its predecessors.
“It starts to compete with the standard strain, and that’s the one that would be of concern,” Swartzberg says—hence the name, “variant of concern.”
As SARS-CoV-2 mutates, researchers are tracking it, building a “family tree” of sorts. As a result, they know that all three variants of concern seemed to have evolved similar, beneficial mutations independently, a process called “convergent evolution” or “parallel evolution.”
“Convergent evolution,” Otto explains, “implies that they’re finding a solution to the environmental challenges they face, and are converged on the same solution.” It’s like they’ve found the same “secret sauce.”
So what specifically is that secret sauce? Scientists don’t know for sure, but they suspect the variants’ boost in transmissibility has something to do with the spike protein, the spike-like structures which cover the surface of the virus and allow it to infect our cells. Each of the new variants independently developed several mutations, including mutations in the spike protein. These changes, research suggests, allows the virus to attach and get inside of our cells “with greater efficiency than the standard strain,” Swartzberg says. “Once it gets in our cells, it produces billions of progeny that can infect more of our cells and can be spread to another person.” (Researchers recently identified seven other variant lineages in the US that share a common mutation that affects the spike protein, though it’s unclear if they too are more transmissible than previous versions, and the research hasn’t yet been peer-reviewed.)
The variants’ rise wasn’t exactly a freak event. We gave it plenty of opportunities to evolve.
As far as RNA viruses go, SARS-CoV-2 mutates relatively slowly. These mutations occur randomly across the genome, but also in a predictable and “clock-like” fashion, Fauver explains. “Every type of virus has its own mutation rate, or what we call a molecular clock.” The variants, however, are running ahead of schedule—B.1.1.7 for instance, has developed about twice as many mutations as you’d expect over the course of a year. “I like to say it had almost two years’ worth of mutations in this one year since it’s been circulating in humans,” Otto says.
How this happened will likely remain a mystery. But scientists do have one well-supported theory: B.1.1.7, they think, came from an individual who was unable to mount a full immune response to it. Studies suggest that if people get infected with COVID while they are on medication that suppresses their immune system (for example organ transplant recipients, whose bodies may otherwise reject the organ transplant), the virus that replicates within their body may end up looking different than if it had replicated in an individual with a fully-functioning immune system. “They’ll sequence that virus over time,” Fauver says, “and find out that it acquires a bunch more mutations than you would expect in a normal transmission event.”
This might sound like a freak occurrence—but not so fast, Otto says. While the variants arose randomly, we also gave the virus plenty of opportunities to evolve by allowing the pandemic to rage out of control. It’s sort of like playing the lotto: your chances of winning Powerball with one ticket are slim to none. But if you purchased hundreds of millions of number combinations, your chance of winning wouldn’t be so slim. “The problem is, there have just been too many cases,” Otto says, “And so with so many individuals across the world infected, the chance that the virus will get this ‘acceleration’ goes up.”
“You have bad luck when you have bad habits,” she says.
Now is the time to double down on protective measures like wearing masks and social distancing.
Again, we don’t fully understand what is giving these new variants a leg up on other variants floating around. “To have a disease that’s transmitting 50 percent more, we don’t even know what makes that possible,” Otto says. “Does it mean that it stays in the air for longer or that it has an easier time getting into our bodies? We don’t exactly know what’s giving it that kind of advantage.” But based on what we know so far, Swartzberg says, the transmission rate likely has to do with the virus’s ability to attach to our cells.
Even with a more transmissible virus, all three experts agree, hope is not lost. “My answer is to continue doing what we know works, which is wearing a mask, social distancing, not spending unmasked time indoors with people outside of your immediate household or your bubble, what have you,” Fauver says.
“My view of it is that if we have more transmissible strains than the standard strains circulating now, it means that we need to double down on everything we do to prevent getting infected,” Swartzberg says, echoing Fauver. For instance, Swartzberg says he’s considering going grocery shopping a little less often and combining trips to the pharmacy. “You just have to be upping the ante right now.”
Vaccinations are also key. The faster we vaccinate, the fewer chances these variants have to potentially spread and evolve. “How can we keep our vaccines working for longer?” Otto says. “We can bring the case numbers down, give evolution less opportunity.” Data is limited, but so far, it seems our vaccines are effective against the new variants, although possibly not to the same degree as with previous versions.
The discovery of the first variant was a lucky accident. But we shouldn’t leave genomic surveillance up to chance.
In the UK, Otto explains, garden-variety COVID tests are designed to detect three segments in the virus’s genome, like identifying a person by looking at three of their fingerprints. But late last year, health officials started to notice that some people’s COVID tests were detecting just two of the sections. As time went on, the odd result became more and more common. It turns out that a variant, which we now know as B.1.1.7, had developed a mutation in the exact segment researchers were already looking.
B.1.1.7 eventually dominated the country. “As a consequence,” Otto says, “they had hundreds of thousands of individual people getting tested for COVID that they could tell, do they have the variant or do they not have the variant? That’s why they have so much information about this variant.”
The spread of B.1.1.7 through England over November and December, with London inset at top-right. pic.twitter.com/fVfL0xijcx
— Theo Sanderson (@theosanderson) January 8, 2021
The UK has also poured tens of millions into conducting genomic surveillance, giving it what Fauver calls the “gold standard” of national sequencing strategies. As of late January, the country had sequenced around 200,000 coronavirus genomes. The United States, on the other hand, a country about five times the size of the UK, has sequenced about half as many genomes, the Wall Street Journal reports. The effort to track SARS-CoV-2 variants in the US is also less centralized, Fauver says, happening on more of an “ad hoc” basis among academic institutions and state health departments.
Since the beginning of this pandemic, the UK has sequenced around six percent of all its cases. The United States has only managed to sequence about 0.3 percent of cases. As a result, Swartzberg says, “We’re blind to what’s happening.”
Without a robust national surveillance program, we’re not only failing to monitor the current variants of concern—but also setting ourselves up to miss future ones, Otto says. “Where are we gonna miss [future variants]? In places like the United States, with many cases and a very low rate of genomic sequencing.”
The success of the vaccine also hinges on our ability to track the variants of concern. Pharmaceutical companies like Moderna and Pfizer/BioNTech are already preparing to supply “booster shots” of their vaccine to combat the new variants. But if we have no idea how widespread the various variants of concern are in our country, these companies will be operating at least partially in the dark. “The more we know, Swartzberg notes, “the safer we are. We’re not going to get out of this pandemic by ignorance.”