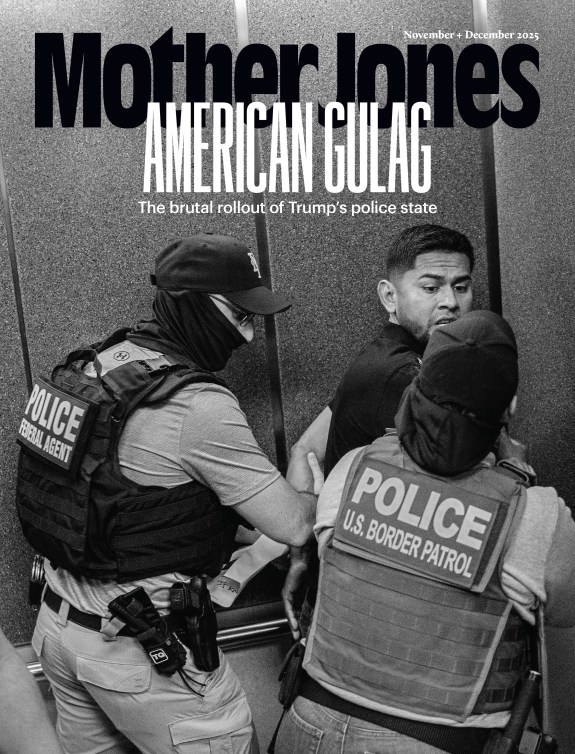
A nursing student from the County College of Morris administers COVID-19 testing for the homeless residents of Newark at the YMCA in Newark, New Jersey. Brian Branch Price/Zuma
For 12 years, Berlyne Vilcant has worked for the city of Newark, New Jersey, as a disease investigator, which means that when there’s a cluster of cases of a particular disease—salmonella at a restaurant, say, or norovirus in a hotel—it’s her job to figure out how it started, who caught it, and how to stop it from spreading further. A lifelong Newark resident, she grew up in a family of Haitian immigrants, and even as a child knew that she wanted to work in health care. As a teenager, inspired by the character of a restaurant health inspector in the 2003 movie Deliver Us from Eva, she decided to go into public health.
In January, Vilcant was busy with run-of-the-mill outbreaks: hand, foot, and mouth disease at a daycare, Legionella at a senior center, isolated cases of giardia. When she told her friends that she was worried about a new virus tearing through China, they reassured her. Don’t worry, they said, it won’t come here. But as Vilcant read more reports, she remembers thinking, “Oh my gosh, if it arrives in the United States, I know I will not have a life.” On Saturday, March 14, her supervisor at the health department called to tell her that someone in Newark had tested positive for the virus. “My heart fell to the floor,” she recalls. “From that moment on, I knew that this was something that was going to be serious, and we needed to treat it as if it was going to be here for a very, very long time.”
Over the next two months, Vilcant watched her worst nightmare come true, as the virus took hold of her city. On the peak day of April 6, there were 162 positive test results. Local hospital intensive care units approached capacity. Vilcant and her colleague were the only two disease investigators employed by the city, and there was no way that the two of them could call every person who tested positive for the coronavirus. The health department had to bring in seven restaurant inspectors to help. Vilcant’s premonition about work taking over her life proved correct: As the city’s lead disease investigator, she worked 6 a.m. to 11 p.m. seven days a week. She rarely saw her two school-aged children.
During those frightening days, it sometimes seemed to Vilcant as if the long hours weren’t even making a difference. All around her, people were sick and dying. Sometimes, when a member of her team called someone to tell them that they had tested positive for the virus, the reaction was hostile. How dare she imply that their family had let the virus in? Even those who wanted to cooperate sometimes couldn’t. In Newark, where 28 percent of residents live below the poverty line, staying home for two weeks was out of the question for many. As the pandemic wore on, it became clear that Black and Latino people were especially likely to suffer severe cases and die from the virus—these two groups make up 86 percent of the city’s population.
In the battle against the coronavirus, Newark faced long odds. Yet about two months into the pandemic, something astonishing happened: Cases in the city began to decline. The trend continued: By early May, there were 50–60 cases most days, by June, the numbers fell to the 20s. This was remarkable, especially given the city’s proximity to New York City, where the virus was still raging.
Perry Halkitis, dean of the School of Public Health at nearby Rutgers University, attributes the city’s early success to a combination of factors: Newark Mayor Ras Baraka showed strong leadership, briefing the city every day in candid town halls on Facebook Live. The university’s public health school provided expertise and a willing group of students ready to volunteer and work alongside Berlyne and her colleagues. But probably the most important factor, says Halkitis, who helped coordinate Newark’s pandemic response, was the city’s investment in a particular strategy.
During an outbreak, infectious disease circles have a mantra: Test, trace, isolate. That is, diagnose cases, track down the people who each patient may have exposed, and quarantine people who may be sick until they have a negative test. The strategy, which has been honed by public health workers around the world over several decades, has successfully controlled outbreaks of tuberculosis, SARS, and MERS, and Ebola. As the last six months of the pandemic have shown, implementing that mantra is easier said than done. Most parts of the United States are still struggling with the testing step, much less tracing and isolating. But almost as soon as COVID-19 arrived in Newark, leaders—including the mayor, health department officials, and experts from the Rutgers—mobilized to build a test-trace-isolate infrastructure for the city. “We were all coming together,” said Halkitis. “What was really good for Newark was that all hands were on deck.”
Against the backdrop of the national shortage of coronavirus tests, Newark public health officials strategized about how best to use the small number of tests they had. Other cities’ testing sites were concentrated in affluent neighborhoods, but Dr. Mark Wade, the head of the city’s Department of Health and Community Wellness, made a deliberate decision to make it as easy as possible for people without access to health care to get tested. In the late spring, when it became clear that the coronavirus was especially severe in Black and Brown communities, the health department opened more testing sites in neighborhoods where people of color predominantly live, and made a special effort to reach senior citizens who lived there. Elsewhere in the United States, cities built drive-through testing centers—but in Newark, where many people don’t have cars, the sites took walk-up patients, as well. The city also spent $2 million to set up a facility to test 2,200 homeless people at an airport hotel and to find temporary housing for those who were infected.
Hoping to ensure that they made the most out of each precious test, Newark officials focused their efforts on contact tracing. Because the cash-strapped city didn’t have money to immediately hire a tracing corps, the health department recruited volunteers. By late April, the program was up and running, but city leaders wanted to improve the data collection and put more muscle into the tracing effort. They looked to nearby Massachusetts, whose innovative tracing program—the first and most ambitious in the country—was showing signs of success. The force behind Massachusetts’ program was a global public health organization called Partners in Health, and its tracing method combined carefully trained tracers and a sophisticated data management system. Newark teamed up with Partners in Health and the Rutgers School of Public Health to supercharge its tracing system. In short order, the city trained 400 contact tracers, many of them volunteers from Rutgers.
Many of the lessons that the PIH team learned in Massachusetts proved useful in Newark. For example, they worked with cellphone carriers to make contact tracers’ number appear as “COVID-19 info” rather than “unlisted,” in order to improve the chances that people would answer the call. But there were other, more fundamental challenges that they hadn’t faced in Massachusetts. Setting up testing sites for the most vulnerable people in the city—especially those in the Black and Brown communities—only solved part of the problem.
A more serious one was that many residents were uncomfortable giving out personal information to contact tracers. Some had experienced discrimination at doctors’ offices, so they were naturally wary of sharing medical information with strangers. In Newark, the contact tracers ran the risk of coming off as dispassionate data collectors—workers who were only interested in numbers, not individuals. For that reason, the workers were trained to explain clearly that the information they were gathering would be kept private. They were also trained to listen carefully and to respond with empathy. “It’s not just about data collection,” said Katie Bollbach, the Partners in Health liaison who led the group’s team in Newark. “It’s about ensuring people feel supported and cared for.”
Bollbach, who had worked on Partners in Health’s Ebola response in Rwanda and Sierra Leone before the pandemic, told me that her transition to the United States was jarring, but not in the way you might expect. She was immediately struck by how limited the access to health care many Americans had. In Sierra Leone, one of the poorest countries in the world, most villages had free community clinics, along with workers who traveled door-to-door to check on residents during infectious disease outbreaks. In America, that kind of outpouring of health support was unimaginable. “The emphasis on community-based care as the cornerstone of good public health in Sierra Leone is just really stark as compared to our system here in the United States,” she told me. “Here, we’re focused on health as a commodity, rather than as a human right.”
What Partners in Health learned over many years spent working on outbreaks in Africa was that testing and tracing are useless without the final step of isolating. Bollbach’s team in Sierra Leone found that most people in villages couldn’t afford food and other necessities during the 21-day quarantine period necessary to stop the spread of Ebola. So officials handed out cleaning supplies—gloves, soap, chlorine—as well as groceries, water, and other supplies to families in isolation. At first it was Partners in Health that provided the supplies, then the government took over. In addition to the material supplies, Partners in Health worked with the health department to send workers to check on people in quarantine: How were they doing? Did anyone else in the house have symptoms? These simple gestures increased the level of trust in the health department. They also increased the likelihood that people would finish the quarantine. Regular check-ins, the team found, made people cooped up in their homes feel less alone.
Bollbach and her team brought those lessons to Newark and created support systems for people who had to quarantine at home. One of them was Wendy Pillajo, who lives with her parents, father-in-law, husband, and three-year-old daughter in an apartment in Newark. Pillajo, a medical assistant at an urgent care clinic, told me about her family’s battle with coronavirus. In May, a few days after her mother attended a family get-together, everyone in her household except her came down with COVID-19. The family’s symptoms ranged from mild (her daughter had a fever for a day) to severe—her parents had debilitating chest congestion, muscle aches, and stomach problems. Remarkably, Pillajo, who was tested several times, never had a positive result. A few months later, Pillajo’s mother tested positive again, and again the whole family quarantined for two weeks.
During each quarantine period, workers from the health department called Pillajo’s family every day to check in. They would ask how each member of the family was feeling, and whether anyone needed anything. After Pillajo’s parents’ tests came back positive, they told the rest of the family how to get to a free walk-up testing site. When Pillajo said she might have trouble getting groceries delivered, the city sent hot meals: Chicken, mashed potatoes, cornbread, rice. Pillajo told me she appreciated the groceries, but even more, she was grateful to have someone to ask questions. She was so worried about her father that she couldn’t concentrate on anything else. Through the daily check-ins, “we understood what was going on, and we saw they were getting better,” she said. “That really helped, to know they care about us.”
By August, Newark’s hard work had paid off. There were just a handful of new cases each day, a precipitous decline from more than a hundred a day at the peak in April. As Halkitis walked around the city, he noticed that the culture of public health had taken hold. Citizens wore masks. They kept their distance from one another. They obeyed the 9:30 p.m. curfew. “People are taking this very seriously,” he said.
If the intensive test-trace-isolate strategy has worked so well in Newark and Massachusetts, then why hasn’t it caught on in the rest of the country? Halkitis believes that one reason has to do with leadership. From the very beginning, the Trump administration has provided little in the way of comprehensive and trustworthy pandemic response guidance, and many cities and states were far from coordinated in their actions. In Newark, from the very beginning of the pandemic, Mayor Baraka had the support of New Jersey Gov. Phil Murphy—their plans for controlling the pandemic aligned.
Other cities have not had the benefit of such a unified vision. In New York City, Mayor Bill De Blasio clashed with Governor Andrew Cuomo during the early days of the pandemic—the governor scoffed at the mayor’s suggestion in March that he might need to close the schools. While the leaders bickered, the virus spread unchecked, and by the end of March, New York City became ground zero for the pandemic. In Atlanta, Mayor Keisha Lance Bottoms butted heads with Republican Governor Brian Kemp—he undermined her every step of the way, from loosening the rules for the initial shutdown to suing her over the mask ordinance she enacted. (He later withdrew the lawsuit challenging the mask ordinance.) Today, in a CDC ranking of coronavirus cases by state, Georgia ranks fourth in the nation. State and local leaders have been on their own, forced to navigate their coronavirus plans with hardly any guidance at all from the federal government. As President Donald Trump told governors in April, “You’re going to call your own shots.”
Another problem with test-trace-isolate, says Halkitis, is that doesn’t work right away. There is a tendency, he said, “for a large portion of the American public to want the easy answers.” Indeed, this fantasy is evident in Trump’s insistence on promoting supposed silver-bullet cures like hydroxychloroquine. Again, that kind of thinking extends beyond the current administration. (How many times have you fantasized about what you’ll do when the vaccine arrives?) But in the actual work of infectious disease control, says Halkitis, “This disease requires hard work, and it means that you have to give up some things.”
Joia Mukherjee, chief medical officer of Partners in Health, echoed those sentiments. “What’s a shame is that we as the United States have been totally unambitious” in contact tracing. But she sees Newark as a bright spot: “Newark is a very hard place to work,” she told me. “There’s a lot of poverty. But the Department of Public Health there has the same view that we do at Partners in Health, which is: Protect the vulnerable.”
Vilcant feels a surge of satisfaction when she sees the chart showing the decline in coronavirus cases in her beloved city. By the beginning of September, there were only a handful of cases every day. At these moments, she feels that the hard conversations, the logistical morasses, the 70-hour work weeks—it was all worth it. But the pandemic isn’t over yet, and she knows it would be a mistake to let down her guard. “My investigators and my contact traces are having that mindset to push forward and continue to do the work that they’ve been doing,” she said. After so many months, this is hard. It’s a marathon. Sometimes, Vilcant’s kids tell her that they hate her job because it takes her away from them. “I have to tell them, ‘This is not going to be forever. In the long run, you will understand why mommy had to take a lot of time off from family to devote my time to make sure that this process is done.’”