Harvard Medical School
In Cancer: The Emperor of All Maladies, a three-part documentary executive-produced by Ken Burns and set to air on PBS from March 30 to April 1, director Barak Goodman delivers a sweeping (and fascinating, and tear-jerking, and horrifying) history of the science, politics, and culture of the disease we fear most.
The film, based on the Pulitzer Prize-winning book by Columbia oncologist Siddhartha Mukherjee, escorts viewers from our dismal past into a more-hopeful modern era in which genomics and big data promise actual breakthroughs after decades of crushing defeats and blunt-force treatments ranging from poisoning (chemo) to radical mastectomy.
Goodman, whose previous work has earned him two Emmys and a Oscar nomination—that was in 2001, for Scottsboro: An American Tragedy—introduces us to contemporary doctors and patients coping with the vast gaps that remain in our understanding of the disease, as well as to the historical figures who had the most profound impact—for good and for ill—on the lives of the stricken. Watch the trailer first, and then we’ll chat with the director.
Mother Jones: What drew you to this history? Have you been personally affected?
Barak Goodman: My beloved grandmother died of colon cancer when I was 20. I remember it being very traumatic. It’s one of the most avoidable kinds, but they caught it late and she died very suddenly. So that was lurking in the background, but the proximate cause was I got a phone call from WETA, expressing their interest in making the book into a film. The book is really a wonderful piece of work. It opened my eyes to a lot of things.
MJ: How would you rate our success in the so-called war on cancer?
BG: Certainly it’s been a failure if you hold it up to its own expectations. At the time they declared it, in 1971, the goal was to solve the problem within a decade or less. Mortality rates now are down somewhat, but not strikingly so. But in terms of our understanding of what cancer is and what the cancer cell is, it’s been a huge success. It’s striking how little we knew then. In the film, people say it was compared with going to the moon, only that was much easier because we knew how to get to the moon, we knew where the moon was. In this case we knew next to nothing. A lot of progress has been made, and we’re really poised to translate that knowledge into therapies, so knowledgeable people are quite optimistic.
MJ: And yet cancer has always proved unexpectedly elusive.
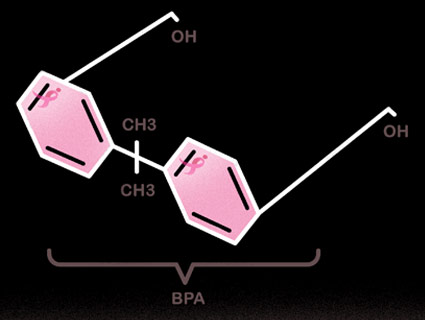
BG: Unbelievable! It is the most devilishly complicated, resilient disease—set of diseases—that is possible to imagine. First, it’s harnessing the very forces that give us life—it’s life unleashed, in a way. To defeat it without killing you is very difficult. The second thing is, it changes so fast, mutation upon mutation, and it becomes not a single target but 100. Figuring out how to combat it with any one drug or any set of drugs, for most kinds of cancer, is almost impossible.
MJ: Chemotherapy works well for childhood leukemia, but not much else. It strikes me as incredibly primitive. You’re literally poisoning people hoping it’ll kill the cancer before it kills the patient. Some of these drugs can actually cause cancer! Do we know how many people die from their treatments versus how many are saved by them?
BG: That’s very hard to pin down, because it varies from cancer to cancer enormously, and the stage of cancer. But you’re right. Chemotherapy is an incredibly blunt instrument—and yet it still is the predominant therapy. There’s been lots of talk about therapies that are more specifically aimed at what’s wrong with a cancer cell, but really only a fairly small number of those targeted therapies have been developed. As you point out, chemotherapy sometimes extends life a few months, but often not much more—and it’s hellacious to go through.
MJ: We’re essentially using the same treatments we did 30 years ago.
BG: We are. They’re somewhat more effective, somewhat more targeted, and they use them in combinations that make them more effective, but the paradigm is the same. Of course, we haven’t discussed prevention and early detection. The decline of smoking rates alone has had more impact on mortality than anything else by far. So that’s a promising way of getting to cancer.
MJ: Okay, so if everyone quit smoking right now, today, what sort of drop would we see in cancer rates?
BG: I believe 30 percent. We have a quote in the film that if all known prevention methods were put into effect—not only stopping smoking but controlling obesity, less exposure to UV rays, and other things—we could cut cancer by 50 percent right now.
MJ: If you were to graph cancer mortality for nonsmokers over time, what would that look like?
BG: Pretty much flat. It’s a little tough, because you have to correct for an aging population, but when you compare apples to apples from today to 25 to 30 years ago, I think it’d be slightly declining. Early detection has had an impact on breast cancer [death] rates and certainly colonoscopy has had a huge impact on colon cancer. Vaccinations have had a huge impact on cervical cancer. But overall it’s a pretty flat chart, and that’s disturbing after spending billions of dollars. But if you stop the clock right now, it doesn’t account for the undercurrent of basic science that’s set us up for much more rapid advances in the next 30 years. I’m not trying to be Pollyanna-ish. With a couple of exceptions, every major researcher feels we’ve turned a corner.
MJ: But people have been saying things like that for decades.
BG: Yes, but that’s deceptive. As Sid [Siddhartha Mukherjee] says at the end of the film, there’s this superficial cycle of optimism followed by crushing disappointment all through the history of cancer. From radical surgery to chemotherapy to targeted therapy, it happens again and again. But what that discounts is a steady upward trajectory in knowledge. Already, immunotherapy, probably the most exciting new avenue of cancer therapy, is making a significant difference. These clinical trials are extremely promising for a certain subset of cancers.
MJ: What about all of the other cancers?
BG: The most common cancers are also the hardest to attack with conventional therapies. All the smoking-related cancers, including lung and kidney cancer, and also melanoma, have too many mutations to target with drugs. On the other hand, those cancer cells look very different from healthy cells and are more vulnerable to immunotherapy. So immunotherapy may have the easiest time with the most complicated cancers, and those caused by the fewest mutations are probably the ones for which we’ll develop targeted drug therapies. The ones in the middle are going to be the biggest problem.

MJ: Your film really underscores the hubris of the medical profession—the jealous guarding of clinical turf against emerging facts. It covers, for example, how radical mastectomy was developed on the false assumption that cancers grow in an orderly pattern. Will you talk about what happened when Dr. Bernard Fischer challenged that prevailing dogma?
BG: With radical mastectomy there was a very logical assumption that the more you cut out, the more lives you save, but it was never subjected to clinical trials. In fact, there were no such thing as clinical trials when it was first developed. As Sid says, these half-truths become full truths in peoples’ minds, and the mere suggestion that they’re wrong triggers a hysterical reaction.
Bernie Fischer just had a very independent streak and was not someone who accepted received wisdom without question—and he was tough enough to undergo the bruising that happened when he proposed clinical trials on radical mastectomy. He was cut off from his grants. He was vilified. He was ostracized. He didn’t care! It takes someone like that to puncture these entrenched ideas.
MJ: Millions of women owe a debt to that guy.
BG: Huge debt! He is one of the real heroes of the cancer story. They’re few and far between.
MJ: Would breast cancer treatment have developed differently had it mainly affected men?
BG: Without a doubt. As Rose Kushner says in the film, nobody would cut off a man’s limb without his permission while he was asleep, but if it came to a woman’s breasts, they did it all the time. There was this paternalistic attitude—a kind of disregard for the notion that women’s breasts might be important to them in some way other than to feed children. It took not only Bernie Fischer, but the activism of women with breast cancer to overturn that. I think it’s no accident that breast cancer has triggered the most intense activism of any kind of cancer. It’s these women who have underwent the worst, most disfiguring, most debilitating kinds of treatments.
MJ: Also, now, when you put a promising new cancer drug in clinical trials, you get a lot of people saying, “I don’t want to be in a randomized trial, I just want the drug.” Will you reflect on the ethics of that situation?
BG: It’s a difficult problem. This cycle of optimism followed by disappointment—the only solution is to subject these things to disciplined trials. In the case of Herceptin, Genentech responsibly resisted opening its trials to lots of women who simply wanted the drug. As [then-CEO] Art Levinson says in the film, you want to be able to look people in the eye and say, “I know this drug can help you,” and you can’t do that without a clinical trial. As harsh as that may seem, it’s the best way of determining efficacy. We have a scene with parents of a little girl who are weighing whether to enroll her in a clinical trial and they’re struggling with the idea that a computer is gonna randomly pick the treatment their child gets. It’s very hard for people to accept, but it’s scientifically necessary.
MJ: Knowing everything you know, how do you suppose you would approach treatment if you were diagnosed?
BG: I ask myself that all the time. I think I would probably try anything, simply because you hear these stories of miracles. They do happen. I was just with a woman the other night who had stage four metastatic melanoma, which was 100 percent fatal until recently. She was told she had months to live and she decided to take one more step and enroll in this immunotherapy trial at Memorial Sloan Kettering. Now she’s three years cancer-free with prospects of living a normal life. I certainly don’t judge anyone who decides not to do that. I admire, in a way, people and doctors who accept the overwhelming likelihood that you won’t be cured. But I probably would take the chance.
MJ: I’m still trying to get a handle on whether chemo even helps people, other than kids with Leukemia.
BG: The problem is, chemotherapy is a one-size-fits-all solution but cancer is different for every person—literally. I don’t understand all the intricacies, but it’s very hard to say, “You’re gonna benefit from chemotherapy, and you’re not.” You kind of gotta try it. One of the promising avenues of research, by the way, is getting a better sense for each person which mutations underlie their cancer. Almost like you’d get a blood test, you’d get a genetic test and then they are able to target those things.
MJ: How long before that’s routine?
BG: Not long at all. If you’ve got the money you can already do that. But the costs of these kinds of genetic tests are nose-diving. I’d say in 5 to 10 years almost everybody will have their cancer sequenced, and then a better set of decisions can be made. Right now they’re still throwing the kitchen sink at people. But that will change.