<p><a href="http://www.shutterstock.com/cat.mhtml?lang=en&search_source=search_form&version=llv1&anyorall=all&safesearch=1&searchterm=antibiotics&search_group=" target="_blank">Ermolaev Alexander</a>/Shutterstock</p>
Lately, I’ve been fascinated by a study on antibiotic prescription rates across the United States that was recently published in the New England Journal of Medicine. The researchers found a surprisingly wide variation among the states, and the rates—expressed in terms of prescriptions per 1,000 people—seemed to follow a geographical pattern: The Southeast had the highest rates, while the West’s were lower. West Virginia had the most prescriptions, and Alaska had the fewest. The rest of the country fell somewhere in between. Here’s a map of the findings:
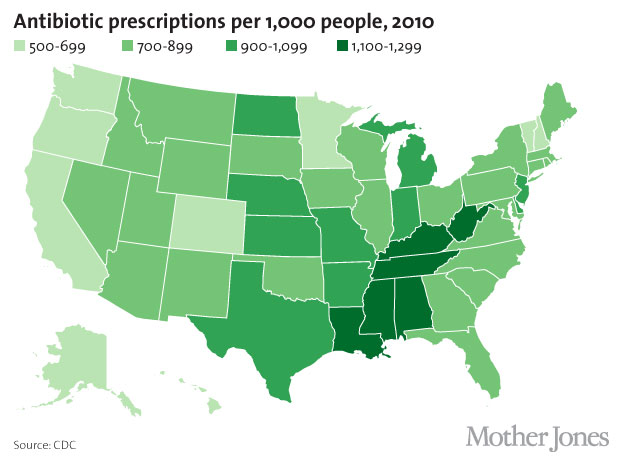
As I thought more about the map, I wondered whether the prescription rates followed any demographic patterns. Lauri Hicks, a lead author of the study and a medical epidemiologist at the Centers for Disease Control and Prevention, told me that her team had initially expected to find certain correlations—for example, higher prescription rates in states with large elderly populations. But that didn’t turn out to be the case. Take Florida, which has a sizable elderly population, but only an average antibiotic prescription rate.
Yet Hicks’ team did find one very strong correlation: The states with higher rates of antibiotic use also tended to have higher obesity rates. Take a look at this map of obesity rates by state and see how it reflects the antibiotics map above:
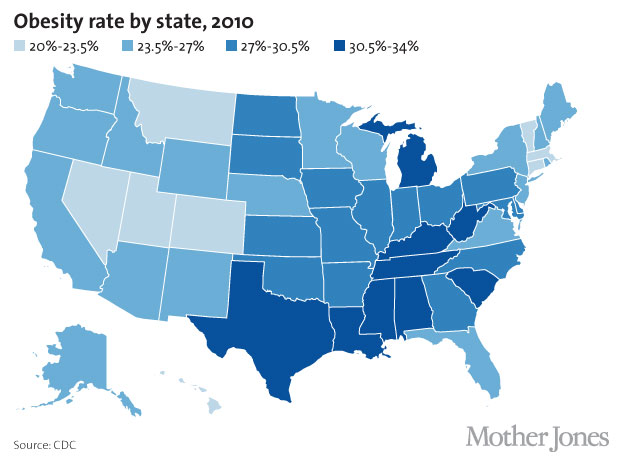
When we mashed up the data behind these maps, we confirmed the strong correlation between obesity and antibiotic prescription rates (we got an r of 0.74, for the statistically inclined). We also found a correlation between the states’ median household incomes and antibiotic prescription rates: States with below-average median incomes tend to have higher antibiotic prescription rates. This makes sense, considering that high obesity rates correlate with low income levels. (You can see the data sets for antibiotic prescription rate, obesity, and median household income level here.)
Hicks and her team can’t yet explain the connection between obesity and high rates of antibiotic prescription. “There might be reasons that more obese people need antibiotics,” she says. “But it also could be that antibiotic use is leading to obesity.”
Indeed, a growing body of evidence suggests that antibiotics might be linked to weight gain. A 2012 New York University study found that antibiotic use in the first six months of life was linked with obesity later on. Another 2012 NYU study found that mice given antibiotics gained more weight than their drug-free counterparts. As my colleague Tom Philpott has noted repeatedly, livestock operations routinely dose animals with low levels of antibiotics to promote growth.
No one knows exactly how antibiotics help animals (and possibly humans) pack on the pounds, but there are some theories. One is that antibiotics change the composition of the microbiome, the community of microorganisms in your body that scientists are just beginning to understand. (For a more in-depth look at the connection between bacteria and weight loss, read Moises Velasquez-Manoff’s piece on the topic.)
Hicks says that more research is needed on the potential connection between antibiotics and obesity. But there are other reasons for doctors to change the way they prescribe antibiotics. As I noted a few weeks back, a recent study in JAMA Internal Medicine found that doctors commonly prescribe antibiotics for symptoms such as sore throat and bronchitis—which don’t usually require the drugs. Considering that bacteria are already evolving to withstand many antibiotics, it’s probably time to figure out how to use them more prudently.