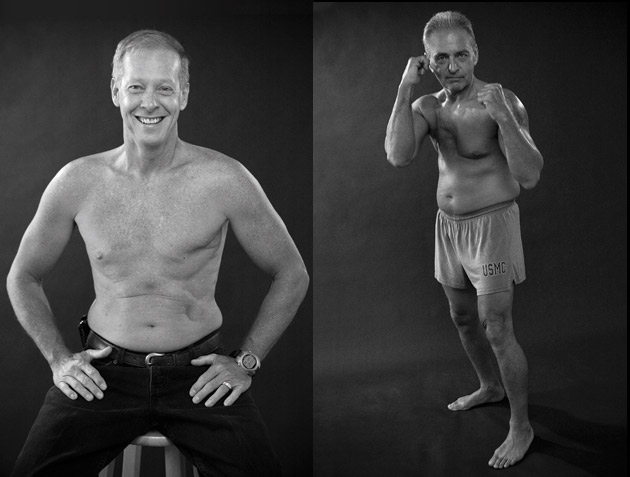
 Kris Thomas (left) and Jim Fontella in the Art beCAUSE breast cancer calendar (David Fox)
Kris Thomas (left) and Jim Fontella in the Art beCAUSE breast cancer calendar (David Fox)
Update, 7/31/12: On Tuesday, the House passed a bill backed by Sgt. Jerry Ensminger and other Camp Lejeune cancer advocates that will help former Marines and their family members get treatment for conditions linked to carcinogens present at the base. The bill has already passed the Senate, and is expected to be signed by President Obama.
It all started with Mike Partain, a.k.a. Number One. A barrel-chested father of four with a goatee and a predilection for aviator sunglasses, Partain was born at Camp Lejeune, the North Carolina base where his father, a first lieutenant in the US Marine Corps, was stationed in the late 1960s. Now he lives in Tallahassee, Florida, where he makes his living as an insurance claims adjuster.
Five years ago Partain’s wife noticed a grape-size bump next to his right nipple. “I thought it was from an ingrown hair or something. I blew it off,” he recalls. But a couple of weeks later he decided to get it checked out. When his doctor ordered a mammogram, he remembers, “a chill went down my spine.” Then came a sonogram: Partain watched in amazement as an image emerged on the screen looking like one of the globular star clusters he knew as an astronomy hobbyist. “I never even knew men could get breast cancer!” he says.
Indeed, it’s rare. For every 100 women with the disease, just one man is diagnosed—and typically around age 70. Partain was only 39. He would undergo a full mastectomy and eight rounds of chemo, leading to gonadal failure—an inability to produce testosterone. “I kept thinking, ‘What did I do to win this lottery?'” Partain told me. “I never drank or smoked. I liked backpacking and Boy Scouts. There is no history of breast cancer in my family.”
Not long after he got the bad news, his father called and told him to turn on the TV. There was a news report about toxic chemicals in the drinking water at Camp Lejeune—and their possible links to leukemia and birth defects. It was the first time either man had heard about the contamination. “I knew right away I’d been exposed,” Partain says. “I figured if this was the cause of my cancer, I wouldn’t be the only one.”
He decided to go public with his diagnosis—no easy deal for the son of a Marine. After Partain was interviewed for a local newscast, he got a call from an Alabama preacher who was raised in the same neighborhood on the base at around the same time. He also had breast cancer. The preacher became Number Two.
Hitting the internet, Partain promptly came across a photo of a man in Michigan—Number Three. “His chest was half gone,” Partain recalls. “His Marines jacket was draped over his arm. I was like, ‘Holy shit!'” Within a year, he’d tracked down 20 men with breast cancer who’d lived or served on the base. CNN aired a story about the group, and another 20 contacted Partain practically overnight. He set up a spreadsheet to keep track of them. Their number slowly grew: 50…60…70. At last count, there were 77.
Partain’s recordkeeping may well prove important, not just for the men—who want answers about their pasts and their destinies—but for researchers seeking insights into the murky environmental causes of breast cancer. From this rare group of men afflicted with an all-too-common disease, scientists might finally get some answers. “We stick out like a sore thumb,” says Partain.
 From top: Mike Partain’s dad (middle row, fourth from right) at Camp Lejeune, 1967; Partain’s mother, Lisette, with her newborn; Sgt. Peggy Price, who served at Lejeune in the ’80s, after removal of a lemon-sized brain tumor; Dewayne Young and his family at Lejeune—”We were always sick,” says his son; Young shortly before his death from adenocarcinoma.People don’t live at Camp Lejeune, they live “aboard” it, which kind of makes sense. The coastal base is built on a series of linked wetlands and aquifers, with the lazy New River meandering through it all en route to the Atlantic Ocean. It’s also massive, covering 244 square miles and hosting some 137,000 Marines, family members, and civilian employees.
From top: Mike Partain’s dad (middle row, fourth from right) at Camp Lejeune, 1967; Partain’s mother, Lisette, with her newborn; Sgt. Peggy Price, who served at Lejeune in the ’80s, after removal of a lemon-sized brain tumor; Dewayne Young and his family at Lejeune—”We were always sick,” says his son; Young shortly before his death from adenocarcinoma.People don’t live at Camp Lejeune, they live “aboard” it, which kind of makes sense. The coastal base is built on a series of linked wetlands and aquifers, with the lazy New River meandering through it all en route to the Atlantic Ocean. It’s also massive, covering 244 square miles and hosting some 137,000 Marines, family members, and civilian employees.
At first impression, the place seems like a glorified summer camp. Signs posted along its main drags point to archery and bowling. But farther out are the Fortified Beach Assault Area, the Flame Tank and Flame Thrower Range, the (former) Live Hand Grenade Course. These places, and dozens of others, are sodden with a witches’ brew of volatile organic solvents and industrial toxins. In 1989 they were added to the federal National Priorities List—basically Superfund sites.
Beginning in the 1950s, for more than three decades, the worst of Lejeune’s contamination intermingled with its water supply. An estimated 750,000 people regularly drank the water, bathed and swam in it, and inhaled its vapors. At Hadnot Point, where the 2nd Maintenance Battalion fixed tanks, jeeps, and other fleet vehicles, storage tanks quietly leaked more than a million gallons of gasoline, forming an underground plume more than 100 feet deep in places, and nearly as big as the National Mall. Through it all pumped Well No. 602, which provided water to thousands of people on any given day. In late 1984, when the military started routinely testing Lejeune’s wells, No. 602 clocked in with 76 times the federal limit for benzene, a carcinogenic gasoline additive. Heavy-duty chlorinated solvents also flowed freely at Hadnot Point, notably perchloroethylene (PCE) and trichloroethylene (TCE)—a known human carcinogen that workers used to degrease machinery before dumping or burying the waste at a disposal site up the road.
Dewayne Young, who worked as a mechanic in Lejeune’s motor pool, died of adenocarcinoma (glandular cancer) in 2010 at age 58. “He said they had them use that one solvent for everything—cleaning anything they were working on, washing their hands with it,” recalls his son, Jeremy Young, who lived with his family on the base during the 1970s. “I can still remember the horrible smell of the water. You couldn’t drink it, it tasted so bad. On top of that, Mom wouldn’t let us. She mostly boiled it and made tea from it, and the tea still tasted funny.”
Two other wells, TT-23 and TT-26, sucked up PCE waste from a nearby dry-cleaning business that catered to the troops. Although the brass knew about some of the contamination as early as 1980, they didn’t close any wells until 1984 and 1985. By that point, wells were coming back with TCE readings as high as 1,600 parts per billion—320 times the current federal limit. The tap water at one elementary school on the base contained 1,148 ppb, which was four times the worst readings in Woburn, Massachusetts, the town immortalized as a poster child of toxic drinking water in the bestseller A Civil Action. While the contamination at Lejeune varied by location, water from numerous wells was combined at centralized treatment plants on the way to offices, barracks, hospitals, and the residences where military families raised their children.
In addition to being the “Home of the Marine Expeditionary Forces in Readiness,” Camp Lejeune now enjoys the distinction of having hosted what is arguably the most contaminated public drinking water supply ever discovered in the United States. It may also be the common thread uniting what appears to be the biggest cluster of male breast cancer cases ever identified.
In 2006, Boston University epidemiologist Richard Clapp got a phone call asking if he’d like to serve on an advisory committee being set up to help the federal government study the chemical exposures at Lejeune. He was an obvious choice. Back in 1980, Clapp had put together the Massachusetts Cancer Registry in response to a childhood leukemia cluster emerging out of Woburn. “I thought, ‘Wow, this is going to be something to watch,'” he says of Lejeune. “That kind of massive exposure, with so many people passing through there, and levels a lot higher than what we saw at Woburn.”
Epidemiology is considered a blunt instrument of science. Most suspected cancer clusters are not what they appear to be—or if they are, it’s tough to prove. They get dismissed as statistical anomalies or phantoms dreamed up by victims desperate to explain what caused their illnesses. Usually the numbers are too small to work with, the exposures too hard to nail down. “You know you have a catastrophe when even epidemiology can detect it,” says Clapp.
Even when local cancer rates do pop out as statistically significant, it’s rarely possible to draw a straight line between environmental exposure and disease the way you can in the lab. (Our proof that radiation causes breast cancer came courtesy of that large-scale public health experiment known as the atomic bomb.) Some 200 different chemicals have been linked to mammary tumors in animals and people, but you can hardly lock human subjects in a lab and feed them TCE or benzene to see what happens.
Yet in a sense, Lejeune is that lab. As Clapp notes, the numbers are huge: hundreds of thousands of men, women, and children exposed to contaminated water. What’s more, the military has precise records of who lived where and for how long. In some cases, it may even be possible to pinpoint, down to the trimester, when fetuses were exposed—knowledge useful for tracking developmental defects. Indeed, it was a survey indicating low birth weights that first caught the attention of the Agency for Toxic Substances and Disease Registry (ATSDR), which is now conducting massive health studies at Lejeune.
Partain’s group, Clapp cautions, still might not be big enough to make a slam-dunk case, but epidemiologists are excited by its potential to dramatically advance what we know about the causes of a disease that kills some 40,000 American women each year and is on the rise globally. As it stands, we don’t know much. Last year’s report on breast cancer and environmental factors by the nonprofit Institute of Medicine declared the evidence on chemicals mostly inconclusive. If the Lejeune data is good enough to prove a link between industrial chemicals and breast cancer in the general population, it will be a first. Clapp, 66, stepped down from his teaching position in 2010, but “I can’t retire from this,” he says. “It’s too compelling. This is up there with the classics: Love Canal, Times Beach. History will look back on this as significant.”
 Mike Partain (left) and Teddy Richardson in the Art beCAUSE breast cancer calendar (David Fox)So why might a bunch of macho middle-aged guys be such a gold mine for researchers hoping to reveal the secrets of what is generally regarded as a women’s disease? Like women, men have mammary glands, a vestige of our evolutionary past. Structures called milk lines take shape early in human embryonic development, before our genes throw the switch that differentiates males from females. But men are far simpler to study than women. Their risk of developing breast cancer isn’t complicated by sex-specific factors such as age of first menstruation, reproductive history, years of breastfeeding, and hormone replacement therapy. And because the disease is so rare in men, a spike in cases is easier to spot. While it’s too early to say anything definitive, Frank Bove, the ATSDR senior epidemiologist leading the Lejeune studies, is impressed both by the number of men on Partain’s list and by their relative youth—the average age of diagnosis is 56.
Mike Partain (left) and Teddy Richardson in the Art beCAUSE breast cancer calendar (David Fox)So why might a bunch of macho middle-aged guys be such a gold mine for researchers hoping to reveal the secrets of what is generally regarded as a women’s disease? Like women, men have mammary glands, a vestige of our evolutionary past. Structures called milk lines take shape early in human embryonic development, before our genes throw the switch that differentiates males from females. But men are far simpler to study than women. Their risk of developing breast cancer isn’t complicated by sex-specific factors such as age of first menstruation, reproductive history, years of breastfeeding, and hormone replacement therapy. And because the disease is so rare in men, a spike in cases is easier to spot. While it’s too early to say anything definitive, Frank Bove, the ATSDR senior epidemiologist leading the Lejeune studies, is impressed both by the number of men on Partain’s list and by their relative youth—the average age of diagnosis is 56.
Last summer I ventured to Wilmington, North Carolina, for a meeting of the ATSDR’s Community Assistance Panel, an advisory committee where experts such as Clapp serve alongside nonscientists like Partain and his friend Jerry Ensminger, a former drill instructor whose daughter, Janey, was raised at Lejeune and died of leukemia at age nine. In 2008, when Congress finally ponied up funding for federal scientists to investigate the illnesses, it was thanks in large part to activists like Partain and Ensminger stirring up holy hell in the media and the halls of government.
Bullish and compact, Ensminger plays Calvin to Partain’s measured Hobbes—though he prefers to say that he and Partain are Meathead to the Marine Corps’ Archie Bunker. “If this is a family, it’s dysfunctional,” he told me. The two men were featured in Semper Fi: Always Faithful, a documentary that aired recently on MSNBC about the Lejeune residents’ battle with the military for health benefits and information about the pollution.
The armed forces, of course, have a long history of making their uniformed ranks sick. There was ionizing radiation from various nuclear detonations, Agent Orange in Vietnam, Gulf War Syndrome, and, most recently, burn pits spewing dioxin and other toxins in the Iraqi outback. In each case, Congress has had to compel the Department of Defense to study the resulting illnesses and offer redress to the troops. At Lejeune, Partain and Ensminger fault the military for shutting down its tainted wells too late, failing to disclose the full extent of the pollution, and denying benefits to sick Marines. To date, Lejeune vets have filed more than 2,100 medical claims, many for illnesses like non-Hodgkin’s lymphoma, kidney and bladder cancer, and cirrhosis of the liver, which have known or suspected links to the solvents found in Lejeune’s wells. The Veterans Administration has approved only 25 percent of the claims it has reviewed.
As the three of us walked through the University of North Carolina campus to the room where the panel was meeting, Partain commented on Ensminger’s cowboy boots. “That’s for kicking some ass,” Ensminger shot back.
True to form, during introductory remarks, Ensminger lit into the Marine Corps for sending only a silent observer to the meeting. Then federal epidemiologist Perri Ruckart rose to deliver a status report: An earlier birth-weight study was being reworked based on new—and more damning—pollution data. Another study was examining the rates of birth defects and cancers among children born at Lejeune between 1968 and 1985. Also in the works was a morbidity study of 300,000 former base residents and workers, focusing on cancer and other illnesses that might be related to the water.
While tens of thousands of women have lived or worked at Lejeune over the years, the extent of breast cancer among them remains a mystery. The morbidity study could reveal whether the numbers—both male and female—are truly out of the ordinary. It is a classic case-control study, comparing a population researchers are interested in with a demographically similar group—in this case, former residents and workers at California’s Camp Pendleton—to determine which group is sicker.
It’s not as easy as it sounds. To get reliable results, you have to enroll huge numbers of people. If only the sick sign up, you’ve got a problem known as selection bias, which skews the results. The Lejeune researchers won’t merely rely on study participants to tell the truth; they’ll laboriously confirm the medical diagnoses.
When these kinds of studies pan out, they can have a major impact on public policy and medical practice. It was case-control studies, for instance, that first reliably linked smoking to lung cancer, resulting in warning labels, class-action suits, and public health campaigns. The Lejeune studies will take years and cost north of $20 million. Cleaning up the base will likely run about 15 times that.
 From top: Allen Ray (left) lived at Lejeune as a child in the 1970s and 1980s, and died of pancreatic cancer at age 38; Lance Cpl. Ariel Cintron was stationed there in the ’70s; Cintron (left) with cancer-stricken comrade Julio Medina, who was also was based at Lejeune, shortly before his death; Cintron at Medina’s funeral; Jerry Ensminger with daughter Janey, who died of leukemia at nine; Ensminger testifying at a House committee hearing.
From top: Allen Ray (left) lived at Lejeune as a child in the 1970s and 1980s, and died of pancreatic cancer at age 38; Lance Cpl. Ariel Cintron was stationed there in the ’70s; Cintron (left) with cancer-stricken comrade Julio Medina, who was also was based at Lejeune, shortly before his death; Cintron at Medina’s funeral; Jerry Ensminger with daughter Janey, who died of leukemia at nine; Ensminger testifying at a House committee hearing.
The most worrisome chemicals found in Lejeune’s water have been used by industries of all stripes. TCE was once a pet food additive, a coffee decaffeinating solution, a wound disinfectant, and an obstetrical anesthetic. And while those uses were banned by the Food and Drug Administration in 1977, the volatile chemical is still employed as an industrial degreaser. Estimates vary, but TCE is thought to contaminate between 9 and 34 percent of the nation’s local water supplies. PCE, with a very similar chemical structure, is still used by most dry cleaners—having replaced TCE for that purpose in the 1950s—and benzene is still added to gasoline, even though long-term exposure is known to “cause cancer of the blood-forming organs,” according to the ATSDR.
Within the past 12 months, after more than a decade of opposition by the military, the Environmental Protection Agency labeled TCE and PCE, respectively, as known and likely human carcinogens. The agency is now in the process of revising its drinking-water standards for TCE, citing toxic effects in the brain, liver, and immune system, not to mention developmental defects, reproductive effects, and kidney cancer.
The little we know about the environmental causes of breast cancer comes from relatively small studies of workers exposed to specific chemicals on the job. And those, it must be said, are all over the map. One of the few general-population studies ever to prove a link between chemicals and cancer came out of Woburn, where researchers concluded that high childhood leukemia rates were caused by TCE and PCE in the water. The number of male breast-cancer cases in Woburn was also unusual, but not large enough to be statistically meaningful.
That’s why scientists are looking so intently at the Lejeune cluster, which continues to grow. “If I take a coin and flip it 10 times and get seven heads, that could be biased by chance or not,” explains ATSDR director Christopher Portier. “But if I flip it 1,000 times and get 700 heads, then I guarantee you it’s not due to random chance. If there are real effects, then they will pop out in these studies where they looked marginal in others. We will do distinctly new science here.”
For regulators, industries, and anyone who has been exposed, the stakes couldn’t be higher. The American Cancer Society currently attributes just 6 percent of all cancers to environmental exposure, but that 30-year-old estimate is based on limited occupational studies. And while major breast cancer organizations concede that there’s no clear evidence that chemicals cause the disease in humans, known nonchemical risk factors account for only about half of all breast cancers. The role of chemicals has been “grossly underestimated,” noted the authors of a recent state-of-the-science report.
“A lot of data do suggest chemicals cause tumors in mammalian systems,” Portier told me. “We have good studies now, for example with identical twins, that suggest the numbers could be as high as 75 percent [of all cancers], if you look at environmental factors broadly to include smoking and nutrition.” Not counting those things, Portier adds, he believes it’s closer to 20 to 25 percent, and not the 4 to 10 percent one sees in the literature. Marion Kavanaugh-Lynch, director of the California Breast Cancer Research Program, is also troubled by the existing evidence in animals and humans. “If we can identify these chemicals now, we can more easily avoid them,” she says.
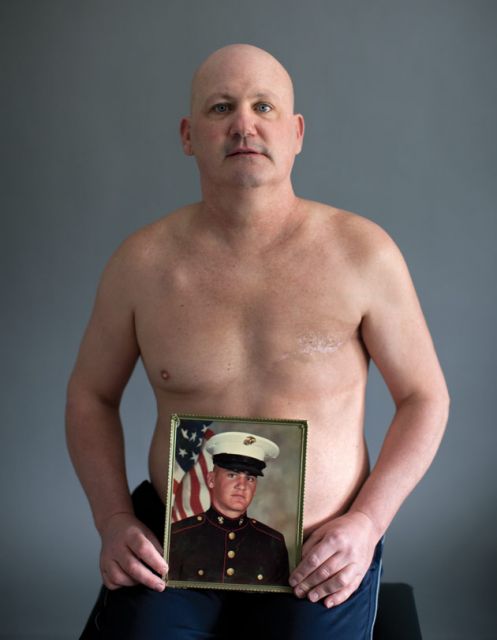 “I felt like a freak,” says Peter Devereaux—”‘How can this be? I’m a Marine, I’m a badass!'”
“I felt like a freak,” says Peter Devereaux—”‘How can this be? I’m a Marine, I’m a badass!'”
(Grant Delin)
It is too late for Steve Martin, Number 23 on Partain’s spreadsheet, who attended a Lejeune day care center built on the site of a former pesticide-mixing facility as an infant—and underwent a double mastectomy as an 18-year-old. It’s obviously too late for the 19 men Partain tracked down who were diagnosed with breast cancer and later died, in most cases after the cancer metastasized. And it’s too late for Peter Devereaux, a.k.a. Number Seven.
A native of Peabody, Massachusetts, Devereaux joined the Marines straight out of high school and was stationed at Lejeune from 1980 to 1982. As a field specialist in the 8th Communications Battalion, he lived in barracks that got their drinking water from the Hadnot Point system. Later, after completing tours of duty in Hawaii and the Philippines, he returned home and found work as a civilian machinist. On weekends, Devereaux earned extra money landscaping and building patios. A serious amateur athlete, he boxed and ran ultramarathons.
Now he can barely walk. Devereaux was so sick that he couldn’t make it to the Wilmington meeting, so I called him at his home in North Andover. In his thick Boston accent, he told me how he was diagnosed with breast cancer in 2008, at the age of 45. “I figured I must have got elbowed playing hoop,” he says of the lump he noticed one day in his chest. “Being a guy, you don’t even know about breast cancer. I never thought men could get it. But I told my wife, and she made me an appointment to see the doctor.”
The verdict was Stage III breast cancer (which would soon spread to his lymph nodes). Devereaux was dumbfounded. “I felt like a freak,” he recalls. “I got no breasts! How can this be? I’m a Marine, I’m a badass, I work out all the time. I ate good, I exercised, stayed fit my whole life, never smoked or did drugs—and you try to figure out how can this have happened?”
Five months after his diagnosis, he received a letter from the Marine Corps at the behest of Congress. It stated that Devereaux might have been exposed to contaminated water while aboard Camp Lejeune, and suggested that he register at a website set up by the ATSDR to identify subjects for its health studies. “When I got that letter in the mail,” he told me, “within one minute it made 100 percent sense to me that contaminated water was how I got breast cancer.” He found a website started by Marines and their families, and was soon in touch with six other men, including Partain. Devereaux agreed to speak publicly in the hope that more Marines might come forward. “I gotta let others know, man. I wish they’d let us know 20 years ago, and it could have been a different result for me.”
Like many men with breast cancer, Devereaux was diagnosed late in the course of the disease. His treatment included a mastectomy and the removal of 22 lymph nodes, followed by radiation and 14 months of chemo. “It beat the crap out of me,” he says. In 2009 he learned that the cancer had spread to his spine, ribs, and hips. “There’s no cure this time.”
Tough guy that he is, Devereaux has found comfort within the very female breast cancer community. “You go into all these pink buildings and places for your mammograms and appointments. You’re this dude, and all these women are looking at you. I meet these women, and they’re so much more open and honest and easy to talk to about emotions. Guys, all we talk about are football, eating, farting, and girls. So they really helped. I felt a burden lifted. I wanted to move forward. My goal now is to raise awareness.”
His combat training hasn’t hurt. Devereaux was more than ready to wage a paper and public relations war against the Marine Corps to secure medical benefits and help other sickened veterans get them too. Vets are covered only for service-related conditions, and he’d been out of the Corps for more than two decades. But last year, after a two-year battle, Devereaux convinced the Veterans Administration that his cancer was as likely as not linked to the water at Lejeune—something only one other vet had managed. (To qualify for benefits, vets must prove beyond “reasonable doubt” that service-related exposures caused their illness.)
Not everyone on Partain’s spreadsheet blames the military. “I can’t say why I got this damned disease,” says Bill Smith, a 77-year-old Floridian who edited the base newspaper for two years in the late 1950s and was later treated for late Stage II breast cancer. “I lived a hard-drinking, fun life. I worked the steel mills in Buffalo. I lived at Camp Lejeune. I don’t know where it came from. I can’t all of a sudden blame the Marine Corps. I don’t know and my doctors don’t know.”
What he does know is that he used to be a swaggering SOB, and that his breast cancer has changed all that. “I’m not what I was,” says Smith, who spent years in advertising after leaving the Corps. “I was a Mad Man. I was a user of women. I’m not even telling you how many times I was married. I’m not a swinger anymore, not a user. I appreciate women now, and they’re so much stronger than men. I went to support groups, I listened to them. I’ve had the privilege of entering a women’s world.”
Many men with breast cancer don’t want to talk about it, but Partain is as chatty as a schoolgirl in spring. It’s why he’s such an effective spokesman. There’s nothing girly about his appearance. He describes himself as “a hairy beasty guy,” and it’s a fair assessment. Not long ago he convinced Devereaux and some of the others to pose for a calendar to benefit breast cancer research.
Yet underneath the affability runs a deep anger. Partain is angry about his cancer, and angry that the Marines haven’t done more to apologize or to compensate the men for their disease. As a journalist, I was allowed to tour Lejeune’s extensive, ongoing cleanup, which involves everything from oil-eating bacteria to soil-vapor extraction to “pump and treat” stations that oxidize volatile organic molecules into less harmful ones. But because he’s a civilian, Partain isn’t allowed aboard Lejeune. This makes him madder still. So before my official tour, he offers to take me on one of his own.
I look over at Partain as we pull into a parking lot just across Highway 24 from the base. He’s wearing shorts and a brown T-shirt that reads “Surf City, USA.” But the tourist attire belies his sour mood. He points to where a chain-link fence and a row of loblolly pine separates the roadway from Tarawa Terrace, his family’s old neighborhood. Next to an entrance gate, four bright yellow pole stubs surround a concrete square the size of a laptop—the now infamous TT-26 well. “They let it pump for 30 years and they poisoned a lot of people,” he says. “Every time I see it, I get angry.”
We watch some gulls fly overhead. “My father chose to have his family here, on that base,” Partain continues, “because when you’re inside the gates of the second Marine Corps division, you’re supposed to be safe. When these people, who are guarding their country, go overseas, and in harm’s way, the last thing on their mind should be, What’s happening to my wife and my kids?
“It’s every woman’s worst nightmare,” he goes on, “that something they do when they’re pregnant can affect their unborn child. I’ve seen it when I talk to the mothers and they learn their child was poisoned. I saw it in my mother’s eyes—the most heartbreaking look, despair, that I’ve ever experienced in my life. I was 39 years old when I saw that look. Part of me wants to go on base and show my family, my youngest daughter. She keeps asking me, ‘Is what’s happening to you going to happen to me, Daddy?'”
Partain pauses, rubbing his hand against the grain of his goatee. “I don’t want these things burning in my head,” he says, “but I don’t want to stick my head in the sand either. I don’t want to forget about it. I have to understand it.”