At first glance, it looked like Greg Perdue was stretching. The 58-year-old sat cross-legged on the matted wall-to-wall carpet in his Aberdeen, Maryland, apartment, a head of shaggy, graying hair bent toward his knees. But when medical examiners gingerly turned him over, they found his bloated face was a deep purple, his nose and mustache covered with crusted blood. Next to a pack of cigarettes on the kitchen table were three clear pill capsules: two empty, one containing an off-white powder that was later identified as heroin.

RELATED: When Using Heroin With a Friend Gets You Charged With Murder
Jessica Pishko
In a former life, Perdue was a mechanic, an avid hunter, a drinker, and a romantic who often drove to the tops of the hills nearby to watch the sunset. After being prescribed painkillers to treat a work injury, he started snorting heroin and became estranged from his friends and family. When the cops found him in April, they determined he’d likely been slumped in his apartment for a couple of days. His was the 113th overdose of the year in Harford County, a white, working-class suburb a half-hour up Interstate 95 from Baltimore. There was no funeral; his ashes sit uncollected at the morgue.
After Perdue’s quiet death, a lanky, affable 38-year-old cop named Brandon Underhill was assigned to investigate the dealer who had sold the fatal dose to Perdue. Underhill, a clean-cut churchgoer who grew out his wavy blond hair and got his ears pierced when he started doing undercover work 10 years ago, quickly zoomed in on a suspect: Zack Carter, a 35-year-old with a rap sheet including several drug charges and an attempted murder. As spring turned to humid summer, he tracked Carter’s cellphone data, talked to “friendlies,” or informants, and met Carter behind the yellow home in J&K Mobile Home Park in Aberdeen, where Carter, whose name I have changed, would lean into Underhill’s car window and exchange glass vials of heroin for cash.
Underhill was surprised to find that Carter was likable, whether he was confidently breaking up neighborhood tiffs or laying into his underlings, whom he paid in drugs or money, if they tried to steal business. After hiding a GPS tracker under the bumper of Carter’s BMW 750, Underhill was able to track the car on his iPad as it traveled to Baltimore a few times a week and then back to Harford to flit among a handful of homes in the county’s housing developments and trailer parks. Meanwhile, overdoses kept mounting: In the wake of Perdue’s death, cops traced 11 back to Carter, none of which were fatal.
The investigation came to a head in predawn darkness four months after Perdue’s overdose, when about 60 officers wearing body armor assembled in an elementary school parking lot for a briefing about the morning’s operation. The high beams of dozens of police cruisers cast an eerie light on the officers—nearly all men—who gathered around Underhill as he laid out the plan: Because Carter spent time in five homes nearby, there would be five simultaneous raids at 5:30 a.m. on the dot. “Everybody in the communities all know each other,” Underhill explained to me as we drove to one of the raid locations. “When noise starts happening, everybody knows.”
The operations that took place a half-hour later looked like a movie scene: the calm of early morning in the trailer parks was interrupted by flash-bang grenades, yelling, the ramming in of doors, cops in perfect V formations with guns drawn. Masked men woke up whoever was sleeping inside and led them out in handcuffs. One resident complained that it was the third time his home had been raided. A half-asleep Carter was hauled out of bed and booked in the Harford County Detention Center.
Read what it took to go this deep on the opioid crisis—and help support our investigative reporting.
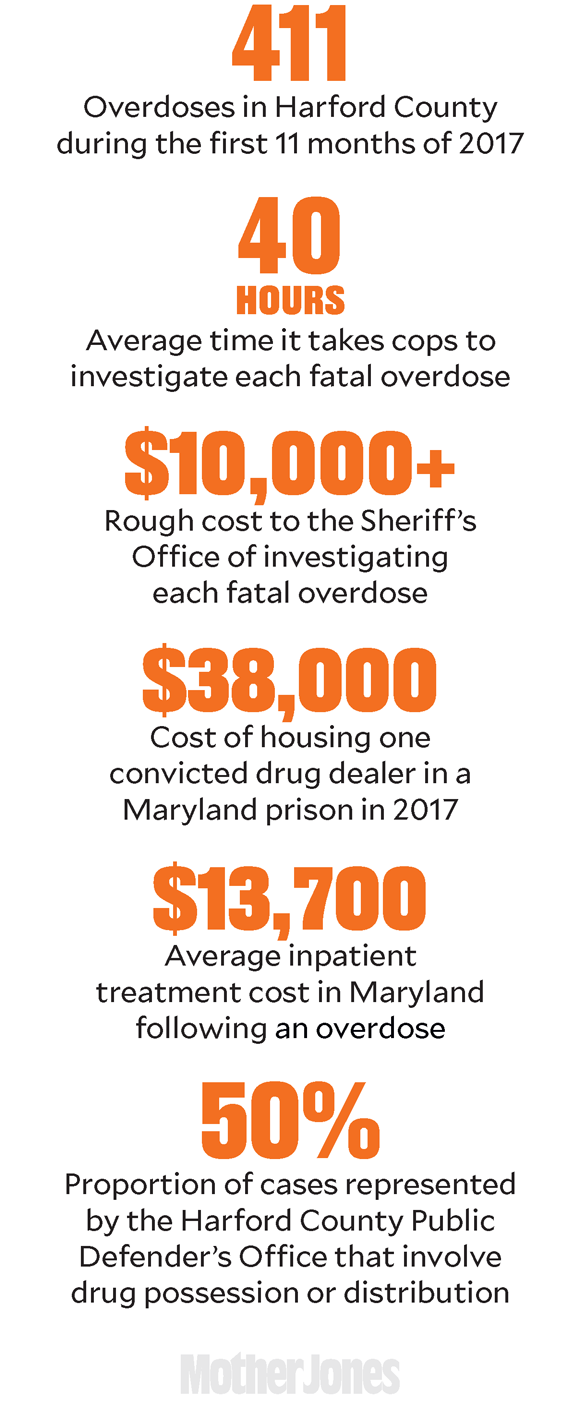
That morning’s raids were part of a Harford County Sheriff’s Office initiative to go after the dealers involved in every single overdose in its jurisdiction, fatal or nonfatal. In each case, the county sends a drug investigator, who treats the place of overdose—be it a car in the Home Depot parking lot or a bedroom in a million-dollar home—as a crime scene with a culprit to track down. The task is monumental: In the first 11 months of 2017, there were 78 fatal and 333 nonfatal overdoses in the county of just 250,000 people. “We’re gonna come at you with the full force of effective law and every resource we have available to us,” said the county’s lead narcotics officer, Lee Dunbar, in a Baltimore Sun video titled “Capt. Dunbar’s Message to Harford’s Drug Dealers.” The county, one of the first in the nation to investigate every overdose case, has served as “a model of what you can do and what you should do,” said Buck Hedrick, supervisor of the Drug Enforcement Administration’s intelligence team in Baltimore.

Undercover detective Brandon Underhill
This approach contributes to the already steep price of the epidemic. The average fatal overdose takes more than 40 man-hours for the county’s narcotics team to investigate, though that number is highly variable: Underhill worked almost exclusively on the Carter case for more than two months. The cost to the Sheriff’s Office of investigating a typical fatal overdose runs between $10,000 and $15,000 once things like salaries, overtime, personal protective gear, and travel to interview witnesses are taken into account. But the spending doesn’t stop there: Transporting, cremating, and burying an unclaimed body costs about $700. Medical treatment runs $13,700 for the average inpatient visit after an overdose in Maryland. Add that to the cost of jail or prison for the dealers (about $81 per inmate per night at the Harford County Detention Center), lawyers representing the dealers (at any given time, roughly half of the county’s public defenders are working on drug possession or distribution cases), and lawyers representing the state (the state’s attorney’s office spends about $500,000 a year prosecuting drug cases). And then there’s the crime fueled by addiction: Harford County State’s Attorney Joseph Cassilly estimates that more than half of all thefts, robberies, and frauds in the county are related to efforts to acquire cash for drugs.
For all the time, energy, and money Harford cops spend cracking down on dealers, overdoses in Harford are skyrocketing. Then again, there’s no blueprint for cops to follow when it comes to an epidemic of these proportions, says David Kennedy, a criminologist who directs the National Network for Safe Communities. After decades of a failed war on drugs, many cops know that arresting users doesn’t work, so they’re focusing on dealers, he says. “The sheriffs are so desperate to try something. There are people dying every day, and they’re on the front lines, and we don’t have anything to offer them right now.”
The truth is that Harford—along with every other US county hit hard by the opioid epidemic—is winging it. “I’ll go anywhere to try and get best practices,” said Harford County Sheriff Jeff Gahler at a press conference announcing the opening of the “H.O.P.E. House,” a model of a drug user’s bedroom on wheels aimed at educating the public about telltale signs of drug abuse. “I don’t mind putting it in reverse if it doesn’t work and backing it up and trying again.”
Both the Obama and Trump administrations have repeatedly acknowledged the need for treatment for drug users. “We’re going to take all of these kids—and people, not just kids—that are totally addicted and they can’t break it,” Donald Trump promised at a Columbus, Ohio, town hall meeting just before the election. “We’re going to work with them, we’re going to spend the money, we’re gonna get that habit broken.” He also promised to declare a national emergency, which would free up federal money to support afflicted communities. Nothing of the sort has happened. Instead, in October Trump declared a public health state of emergency, which opened up a fund containing a grand total of $57,000—or about $1 per fatal overdose victim. As of this writing, neither the Department of Health and Human Services nor the Office of National Drug Control Policy have permanent leaders. Repealing Obamacare or enacting the proposed GOP tax bill would cause millions of Americans with substance abuse and mental health disorders to lose coverage. Meanwhile, the White House Council of Economic Advisers recently estimated that the epidemic cost the nation $504 billion in 2015.
In the absence of federal leadership and funding for social services, police have become the de facto responders, says Keith Humphreys, a Stanford psychiatry professor who advised the Obama administration on drug policy. “If you don’t have health care dollars, what else can you do? Put people in jail.”
Carter was released on bail three days after the raid, charged with 11 counts of drug offenses, and given a court date in December. The state is also considering charging two of his henchmen with second-degree manslaughter. Since the raid in August, there have been five more overdoses in the trailer parks where police suspect the men operated. The cops are, for the most part, used to this game of cat and mouse, but sometimes, Underhill confessed to me, the process can seem futile. “I feel like we’re just playing whack-a-mole,” he said, sounding exhausted. “Sometimes you feel like you’re just banging your head against a wall—because somebody else is going to pop up and take that business.”
Harford County sits squarely between Baltimore and Philadelphia, but it more closely resembles the Pennsylvania Dutch countryside to its north: cornfields and dairy farms dotted with strip malls and cookie-cutter housing developments. The area has long been home to white, middle-class Republicans—lots of cops, military families, and people who commute to Baltimore. The place can have a small-town feel, with high school football and holiday festivals making front-page news in the local paper. On #WantedWednesday, the Sheriff’s Office Facebook account features mug shots of people they’re looking for, typically for things like not showing up in court or failing to pay child support, against Wild West-themed backgrounds.
While Harford’s overdose epidemic is fairly recent, opioids aren’t new to Baltimore. For decades, heroin has plagued the city—especially poor communities of color—inspiring HBO’s The Wire and giving the city the unwanted title of the “heroin capital” of America. “It’s been an epidemic in my town since I can remember,” a Baltimore dealer known as Doc told me. “Growing up, I didn’t even know what dope was, but I knew everybody that sold dope had money.”

Aberdeen, Maryland
Opioids started seeping into the surrounding counties in the mid-’90s, when Purdue Pharma introduced OxyContin and dramatically underplayed its addictive qualities. Thanks to pharmaceutical lobbying, years of liberal painkiller prescribing—the United States consumes more than 70 percent of the world’s opioid painkillers—planted the seeds for widespread addiction to both painkillers and heroin, which is chemically similar to the prescription pills but far cheaper and more potent.
As the demand for opioids grew in suburban areas, capillaries sprang up from the main drug trafficking artery of Interstate 95, which runs from Florida to Maine, bringing opioids to small towns like Bel Air and Aberdeen. But the turning point in Harford—and much of the country—came in 2015 after fentanyl, an opioid up to 50 times more powerful than heroin that is typically manufactured in illicit labs in China, started making its way into the heroin supply. Complicating matters is the fact that, by the time drugs get to Baltimore or Harford County, they have likely changed hands so many times—and mixed with fentanyl and other additives along the way—that dealers often don’t know what they are dealing. Indeed, the customary drug in Baltimore is “scramble”: an amalgamation of heroin and other drugs, sold in gel capsules. “We knew [fentanyl] was coming; we were trying to brace for it,” said Dunbar. He recruited officers to do nothing but heroin investigations, because “we knew we were gonna see this surge.”
Accidental Overdose Deaths per 100,000 Americans
Note: 2016 data is an estimate.
Centers for Disease Control and Prevention
And they did. From 2015 to 2017, overdose deaths in Harford County nearly tripled. Today, the Sheriff’s Office displays the number of fatal and nonfatal overdoses in real time on signboards with running tickers at the county’s police stations and courthouse.
Of course, the epidemic is much bigger than Harford. In Ohio, coroners’ offices use refrigerated trucks to store bodies. In Connecticut, medical examiners’ autopsy caseloads have quadrupled in one year. In West Virginia, 1 in 20 infants are born in withdrawal from opioids. And in Maryland, two-thirds of people in jail have a diagnosed substance abuse disorder, according to a 2016 analysis by the governor’s office. Harford County Sheriff’s Office cops are no longer allowed to test seized drugs suspected to contain opioids on the spot, because of reports that interacting with some variants of fentanyl can be deadly. When the drugs are sent to DEA labs, “while one person is testing, another person is ready to treat them with [the overdose reversal drug] naloxone in case they fall while they’re testing,” says Hedrick, the DEA supervisor.

RELATED: A Brief, Blood-Boiling History of the Opioid Epidemic
Julia Lurie
As the wave of fatal overdoses hit Harford in early 2015, county officials sprang into action. Police officers are now equipped with naloxone and trained that addiction is a disease. Cops on the Narcotics Task Force rarely charge users for drug possession in quantities that seem intended for personal use. After every overdose, cops give victims a “help card” with addiction treatment resources. “We’re not going to solve the problem by putting addicts in jail,” said Underhill. “If they’re not going to get effective treatment, it’s not going to change anything.”
Another part of Harford’s response is aggressively tracking down dealers. In 2016 alone, the county arrested and charged 240 people with felony drug offenses. As Dunbar sums up the strategy, “We need to lock up the bad guys—the dealers and traffickers putting out stuff on the street—but we also play a role in getting the victims help.”
Yet as the opioid crisis continues to metastasize, the line between bad guys and victims is increasingly blurred. “These aren’t two distinct sets of people,” says District Public Defender Kelly Casper. She estimates that 80 percent of the cases represented by her office are drug-related—whether it’s people dealing or stealing to get a fix—and that “darned near 100 percent” of her clients are using. “They want to charge all of these people with drug dealing, when in fact the core of the problem is that they’re users.”
I saw the user-dealer problem play out a few days after Carter was arrested. I was tagging along with Ryan Wolfe, a friendly, middle-aged cop wearing jeans and a Voltron T-shirt who has seen what drugs can do to people—his brother is addicted to heroin. For an hour, Wolfe and I trailed two alleged dealers who appeared to have filled the void left by Carter’s absence. When Wolfe’s team finally pulled them over, he said into his radio, “Let’s hope they still got something, guys.”
Back at the station, five cops wearing masks, rubber gloves, and holsters with guns searched the dealers’ beat-up Mercury Montego. They pulled out a child’s car seat, a Hello Kitty tricycle, a 60-pack of Play-Doh, an Orioles fidget spinner, and an air mattress. One cop slowly poured out family-sized boxes of Froot Loops; another flipped through a child’s drawings of flowers. I noticed, for the first time, a bumper sticker: “My child makes Lisby-Hillsdale a great place to learn.” The dealers, it turns out, were two women I’ll call Vanessa and Tina, a homeless couple, living out of the car and motels, selling to support their own drug addiction.
Later, the women told me how they get by, squeezing an air mattress into the sedan at night, parking in lots where cops won’t arrest them, and occasionally getting a room at the Super 8 to take a shower. Sometimes they pick up odd jobs, cleaning houses or painting. Most weeks, they see Tina’s three young daughters, who stay with their grandmother and believe Mommy’s saving up money for a new house. They take the girls on trips to the park or the library or IHOP—anything cheap.
Both women have been using for the better part of a decade, going through cycles of clean time, relapse, and prison for drug charges. “You use some and sell some—I make my money back to do it for free,” said Vanessa, who started snorting heroin after she was prescribed Percocet for an injury. Tina started just after high school, when a boyfriend introduced her to pills. “It feels like you’re superwoman,” she said of the first time using. “You can run around, get the whole house cleaned, go to work, come home, clean more. And without it you don’t want to do anything. You’re sick.”
It was dark outside by the time the five men, working overtime, had finished searching the Montego. Wolfe’s wife was texting him, wondering if he would be home for dinner. In the end, the cops found a dime bag of weed, and a strip search revealed that Vanessa had slipped a little fold of heroin—enough for a single person to use—in her bra. The officers didn’t press charges. As they were leaving, Vanessa asked Wolfe whether he knew of any local programs that would help her, a felon with a history of drug charges, find a job. She didn’t want to keep living this life, she said. He told her none came to mind.
“Sometimes chalk one up for us; sometimes chalk one up for them,” Wolfe said. “They’ll get another day to do their thing, and we’ll get another day to do ours.”
It’s not that Harford cops don’t empathize with user-dealers. The guy who gets in a car accident is prescribed painkillers, becomes addicted, and then starts selling to support his own habit—“I’ve seen that story 150 times,” Underhill told me. But where do you draw the line? “They’re selling just enough to get theirs,” he said of user-dealers, “but they’re killing people with what they’re bringing back.” He gets most worked up when he talks about the kids: the toddlers strapped in car seats as he pulls parents over for drugs, the children he terrifies when breaking open front doors with Halligan bars in predawn raids, the teens who come home from school to find that cops have gone through their bedrooms looking for drugs.
When it comes to reforming user-dealers, evidence strongly suggests that prison time isn’t very effective. Instead, stable housing, support services, and employment have been shown to promote long-term recovery. Law Enforcement Assisted Diversion, a Seattle program that has been replicated in dozens of jurisdictions across the country, demonstrates the research in action: Rather than jailing people for low-level drug crimes, police divert them to programs offering treatment, housing, and job training. Participants are nearly 60 percent less likely to be rearrested.
The treatment approach also saves money: According to the National Institute on Drug Abuse, part of the National Institutes of Health, “Every $1 invested in addiction treatment programs yields a return of between $4 and $7 in reduced drug-related crime, criminal justice costs, and theft alone.”
“Supply follows demand, not the other way around,” says Lindsay LaSalle, a senior staff attorney at the Drug Policy Alliance. “The war-on-drugs tactics have been wholly ineffective at curbing sales or use—drugs are more available and pure than ever before.”
Attorney General Jeff Sessions is one of the leading advocates for traditional punitive policies, like increasing mandatory minimum sentencing to stop the “thugs and gangs who bring this poison into our communities,” as he told DEA employees in May. “It’s going from today to the 1980s,” says Humphreys, the Stanford professor and former Obama adviser.

A sign in front of the police station in Aberdeen, Maryland, tracks overdoses.
Meanwhile, Trump has proposed gutting the social services that act as a safety net for users and dealers—from job training programs to child care to food stamps. “This is a lot of chicken and egg,” says Marc Schindler, executive director of the Justice Policy Institute. “We need effective substance abuse treatment. People also need jobs. They need adequate education. They need housing.” All of this is, of course, much harder to provide than a prison cell.
Take Doc, the 30-year-old Baltimore dealer who spoke with me under the awning of a McDonald’s across from a corner where he sells drugs. He’d been working these corners for the better part of his life but hadn’t tried opioids himself until he was shot in a drug-related turf war a few years ago and got addicted to Percocet. He found that the drug numbed his pain—of not just the gunshot wound, but also the childhood trauma of growing up on Baltimore’s streets. “Some people done lost their best friend, their brothers, over these fucking corner wars,” he told me. “This shit’s like Iraq.”
When we spoke, he was living in the suburbs with his two kids—daughter loves ballet, son is into football—and waking up at 5:30 a.m. to sell drugs to the early-morning users in the city. He could get a minimum-wage job, he said, but it’s far easier to support his family as a drug dealer than as a McDonald’s cashier. Doc told me he knows how he appears to an outsider: “‘Look at that guy. Gold teeth, pants hanging off his ass.’ You look at us like we’re some kind of monster. Well, look at my school system. If you’re not going to educate me, where am I gonna work?” In August, he told me he had gotten out of prison just a couple of months before. “You think that my kids aren’t fucked up when I’m sitting over in that jail and I’m missing birthday parties?”
Next to Doc under the McDonald’s awning was his friend Dre Jackson, a quieter 39-year-old who’s known Doc for years. Dre, too, had grown up in Baltimore’s rough neighborhoods and had cycled between drug use and prison and recovery. Now, he told me, he was ready to leave the streets behind. He had done a job training program in Pennsylvania—he raved about the peacefulness of the countryside, the lack of violence and drugs—but had come back to Baltimore to take care of his mom. He had a job at a supermarket and a girlfriend who wasn’t into drugs. For the moment, life was good. “I didn’t wanna be out here homeless where all I wanted to think about was getting high.”
When I returned from my trip to Harford County, I called Underhill and asked what had happened to Carter when he was released on bail. After a brief silence, Underhill admitted he had no idea. He’d just come back from a church mission trip to Romania, he told me, and now he was busy preparing for another raid. “It would be nice to try to keep tabs on people,” he said with a sigh, “but we just don’t have time.”
Once or twice a year, Underhill hears from dealers he caught, who call or text or recognize him on the street and tell him that the day of their arrest was their rock bottom, and that they haven’t dabbled in drugs since. “It’s infrequent,” he admitted, but “if it takes all this manpower and two and a half months of effort to get somebody to say, ‘I’m clean, and I’m doing well, and I’m trying,’ then, okay, we’ll keep doing it.”

Baltimore resident Dre Jackson struggles with opioid addiction. “I didn’t wanna be out here homeless where all I wanted to think about was getting high,” he said.
More often, though, he finds out what happens to the people he’s busted another way: by busting them again. In early October, two months after their arrest, Underhill saw Vanessa and Tina hanging out in the trailer park, meeting with the same known drug users they’d been seen with before. When the cops pulled the women over, they found cocaine, a bottle of methadone with the label pulled off, and more than $700 in cash. A strip search found that Vanessa had stored a gram of heroin in her anal cavity. The cops seized the cash, which they suspected was earnings from dealing. The money was “all of our savings to be able to get a place and get off the streets,” the women countered. Once again, because of the small quantities of drugs, the cops let them go.
“It’s very frustrating,” said Underhill. “But I don’t know what to do differently. We can’t just stop.”
And sometimes, dealers disappear. A couple of months after I spoke with Doc and Dre at McDonald’s, I called Doc to check in and kept getting a busy tone. So I called Dre, who told me the news: Doc had been shot and killed in an apparent robbery in September, just a block from where we’d spoken. “I’m still fucked up over it,” said Dre. “I went to the viewing but couldn’t go to the funeral.” It was just too much.
When we spoke a week later, Dre’s words were slurred. He stopped midsentence to start humming. It was his night off, and he and his girlfriend were watching a movie at home. He’d just popped a couple of Percocets, he admitted—my call woke him up from nodding off in the bathroom. “I can’t say I got an excuse,” he said, “but after [Doc] passed away, I’ve been doing it more and more.” This was the same guy I’d spoken to just two months before—the one who had worked so hard to turn his life around. Now it seemed like he was careening off a ledge. Before we hung up, as if he were reading my mind, he said, “Don’t forget about me, okay?”